![]() https://doi.org/10.35845/kmuj.2024.23560 ORIGINAL
ARTICLE
https://doi.org/10.35845/kmuj.2024.23560 ORIGINAL
ARTICLE
Effect of ultraviolet photofunctionalization on implant stability and osseointegration: a randomized controlled trial of UVA and UVC on SLA-coated titanium implant
Naauman
Zaheer ![]() 1,2,
Maliha Shahbaz
1,2,
Maliha Shahbaz ![]() 2,3,
Usman Zaheer
2,3,
Usman Zaheer ![]() 4,
Zainul Ahmad Bin Rajion
4,
Zainul Ahmad Bin Rajion ![]() 5,
Abdul Moeed Zaigham
5,
Abdul Moeed Zaigham ![]() 6,
Muhammad Qasim Saeed
6,
Muhammad Qasim Saeed ![]() 4
4
|
1: Department of Oral Biology, Institute of Dentistry, CMH-Lahore Medical College, Lahore, Pakistan 2: Department of Restorative Dentistry, Faculty of Dentistry, University of Malaya, Kuala Lumpur, 50603, Malaysia 3: Department of Oral Biology, Lahore Medical and Dental College, Lahore, Pakistan 4: Department of Orthodontics, Lahore Medical and Dental College, Lahore, Pakistan 5: Department of Oral Maxillofacial Radiology, Kulliyyah of Dentistry, International Islamic University Malaysia, Kuantan Campus, Malaysia 6: Department of Prosthodontics, Institute of Dentistry, CMH-Lahore Medical College, Lahore, Pakistan
Email
Contact #: +92-321-4440283
Date Submitted: December 20, 2023 Date Revised: October 15, 2024 Date Accepted: October 16, 2024 |
|
THIS ARTICLE MAY BE CITED AS: Zaheer N, Shahbaz M, Zaheer U, Rajion ZAB, Zaigham AM, Saeed MQ. Effect of Ultraviolet Photofunctionalization on implant stability and osseointegration: a randomized controlled trial of UVA and UVC on SLA-Coated Titanium implant. Khyber Med Univ J 2024;16(4):314-21. https://doi.org/10.35845/kmuj.2024.23560 |
ABSTRACT
Objectives: To evaluate the effect of ultraviolet A (UVA) and ultraviolet C (UVC) irradiation on sandblasted, large-grit, acid-etched (SLA) coated titanium implants by measuring their impact on implant stability and osseointegration in the surrounding bone.
Methods: This interventional experimental study was conducted jointly by Combined Military Hospital (CMH) Lahore Medical College and Universiti Sains Malaysia from July 2017 to December 2018, with ethical approval obtained from both institutions. Sixty-six SLA-coated titanium implants (10 mm length, 4.5 mm width) were placed in partially edentulous patients aged >20 years, randomized into three groups: Group A (control, untreated implants), Group B (implants irradiated with UVA), and Group C (implants irradiated with UVC). Implant stability quotient (ISQ) and osseointegration speed index (OSI) were measured using the Ostelltm Mentor device at baseline (day 0), the 8th week, and after 26 weeks of functional loading. Statistical analysis included linear regression and t-tests.
Results: Baseline ISQ levels were 62.1, 65.2, and 69.3 for Groups A, B, and C, respectively. At the 8th week, ISQ levels increased significantly to 77.0, 81.5, and 82.5. Group B (UVA) demonstrated the highest OSI (8.5±3.3), with significant ISQ improvement compared to the control group (p=0.009). UVC irradiation (Group C) showed no statistically significant difference in ISQ compared to the control group (p=0.191). Patients with lower baseline ISQ showed greater improvement across all groups.
Conclusion: Photofunctionalization with UVA significantly enhanced implant stability and osseointegration, suggesting its potential for improving clinical outcomes in dental implantology. Further research is needed to explore the long-term effects of UVC irradiation.
Clinical trial registration number: NCT05467488
Keywords: Implant Stability Quotient (Non-MeSH); Photo Functionalization (Non-MeSH); Ultraviolet A Irradiation (Non-MeSH); Ultraviolet C Irradiation (Non-MeSH); Osseo integration speed index (Non-MeSH); Resonance Frequency Analysis (MeSH).
INTRODUCTION
One of the primary goals of modern dentistry is to restore patient's aesthetics and functionality effectively. Biocompatible titanium implants have emerged as the best alternative in restorative dentistry for replacing missing teeth.1
Osseointegration serves as a critical measure of implant stability. Early implant failure is more frequently observed in younger patients receiving mandibular implants, while delayed failures are more common in the maxillary bone.2 Bone density, as assessed through CBCT, correlates strongly with implant stability and insertion torque values.3 Implant success, in terms of stability and surrounding bone healing, can be effectively and non-invasively assessed by measuring the implant stability quotient (ISQ).4 Implant stability is categorized as either primary (mechanical) or secondary (biological). Primary stability depends on factors such as insertion torque, drill accuracy, bone quality, and implant dimensions. Secondary stability, also known as biological stability, develops over time as a result of osseointegration. Both types of stability are critical for the short- and long-term success of dental implants. Changes in ISQ values are directly correlated with implant stability, where a decrease in ISQ indicates a poor prognosis and potential implant failure.5
The osteoconductivity and bioactivity of dental implants can be significantly enhanced through the application of ultraviolet (UV) light.6,7 Photofunctionalization of implants prior to placement has greatly improved the predictability of successful outcomes in areas with minimal bone density. This process promotes osseointegration by recruiting osteogenic cells, thereby enhancing the biological integration of the implant.8 Additionally, the use of ozonated water has shown promise in improving diseased gum tissue, further supporting the overall success of dental implant procedures.9
Ultraviolet light-facilitated photofunctionalization of titanium implants has gained considerable attention for its ability to enhance the biological activity and osteoconductivity of titanium fixtures.10 The combined bioactive and physicochemical properties resulting from this process are collectively referred to as photofunctionalization. 11 In clinical practice, areas with compromised bone quality are frequently encountered. Photofunctionalization has significantly improved implant success in such cases by increasing the osseointegration speed index (OSI), thereby enhancing implant stability. Notably, unloaded photofunctionalized implants have demonstrated no adverse effects during the initial healing stages of the surrounding bone, compared to untreated implants.12,13
In vitro studies have shown that UVC irradiation enhances hydrophilicity on sandblasted acid-etched (SLA) coated implants more effectively than UVA irradiation. 14,15 Animal studies and clinical trials have also reported favorable outcomes following the insertion of photofunctionalized titanium implants in compromised bone areas, even when using immediate loading protocols.16 Furthermore, UVC has demonstrated a stronger host response, including improved bone density as observed radiographically, compared to UVA.17 Implant failure rates have been significantly reduced by decreasing healing times and promoting osseointegration, even in cases where primary stability was sufficient at placement.13,18
Photofunctionalization of titanium implants and titanium mesh in aesthetic zones has also shown promising radiographic evidence of bone growth around the implant.19 However, despite the growing body of research supporting the beneficial effects of UV light on implant stability, limited evidence exists regarding the most effective wavelength of ultraviolet radiation for achieving optimal implant outcomes.
This study was planned to address this gap by investigating the effects of UVA and UVC irradiation on SLA-coated titanium implants. It explores the novel approach of irradiating these implants with specific wavelengths using UVA and UVC lamps and measuring their impact on implant stability and the surrounding bone.
METHODS
This interventional experimental study was a collaborative effort between CMH Lahore Medical College, Lahore-Pakistan and Universiti Sains Malaysia. It was conducted in the Prosthodontic Department from 1st July 2017 to 30th December 2018, with ethical approval obtained from the Ethical Review Committee of CMH Lahore Medical College, Institute of Dentistry (32/ERC/CMH/LMC), and the Human Research Ethics Committee of Universiti Sains Malaysia (USM/JEPem/17060290). The study was registered as a clinical trial (NCT05467488).
After obtaining informed consent, sixty-six SLA-coated titanium dental implants (DIO, Korea) were placed in patients, recruited through the Prosthodontic OPD. The inclusion criteria included systemically healthy patients aged >20 years with at least one missing tooth, requiring implants to replace single or multiple missing teeth following a minimum healing period of 5 months. Both maxillary and mandibular posterior regions were included, and preoperative CBCTs were used for assessment.
Patients were randomly assigned to three groups (n=22 each) through block randomization using a lottery method (drawing cards). G Power software was used to determine the minimum sample size required for this analysis. The central and non-central distribution protocol of power analysis was selected along with the F-test family. The ANOVA: Fixed effects, omnibus, a one-way statistical test was used. The input had effect size f= 0.4, α err prob= 0.05, Power (1- β err prob) = 0.8 in 3 number of groups. The out for no centrality parameter λ= 10.5600000, critical F= 3.1428085, numerator df= 2, denominator df= 63. A total of sixty-six sample size was obtained with actual power of 0.8180744. 20 Thus, sixty-six SLA-coated titanium dental implants (length, 10 mm; width, 4.5 mm) were selected for placing in the mandible or maxilla alveolar bone. Implants were also randomly divided into three groups (n = 22): Group A, control group, and groups B and C, photofunctionalized for 10 min with UVA (382 nm, 25 mW/cm2) and UVC (260 nm, 15 mW/cm2) irradiation, respectively, by placing samples in UVACUBE 100 (Honle, Germany). The sampling technique used was purposive sampling.
Surgical procedure: DIO dental implants are inserted in the respective osteotomy site prepared with the surgical drill after detailed clinical and radiographic assessment. The surgical procedure involved using local anesthesia (benzocaine 20%) to make the procedure pain-free. A full thickness mucoperiosteal flap was raised in maxillary and mandibular posterior region planned for implant placement. 21
Group B patients receive titanium SLA coated dental implants photofunctionalized for 10mins with UVA lamp (wavelength 382nm, intensity 25 mWcm2). Group C patients receive dental implants pretreated with UVC lamp (wavelength 260 nm, intensity 15 mWcm2). Group A patients receive untreated dental implants. All the dental implants were photofunctionalized with UVA CUBE 100 (Honle). Bone level implants were used, later loaded with adequate size abutments. Insertion torque and ISQ measurements are assessed through Ostelltm Mentor device.
Sutures were removed after one week. Patients were recalled after eight weeks for ISQ and OSI measurement and final prosthesis. Reading was compared for the three groups. Final evaluation done at twenty sixth week mark. CBCT radiographic assessment was again immediately obtained after placing the fixture to determine baseline and repeated during follow-up before (8 weeks) and after (26 weeks) functional loading. All recorded images were saved locally and transferred into the Romexis software.
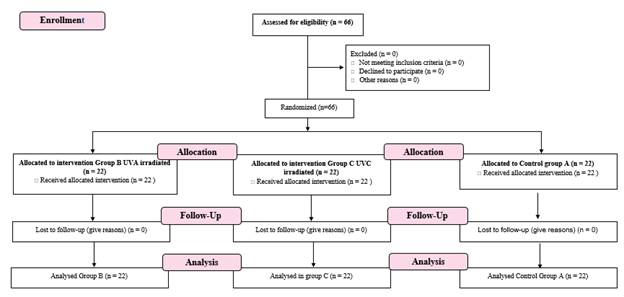
Figure 1: Flow diagram of the study
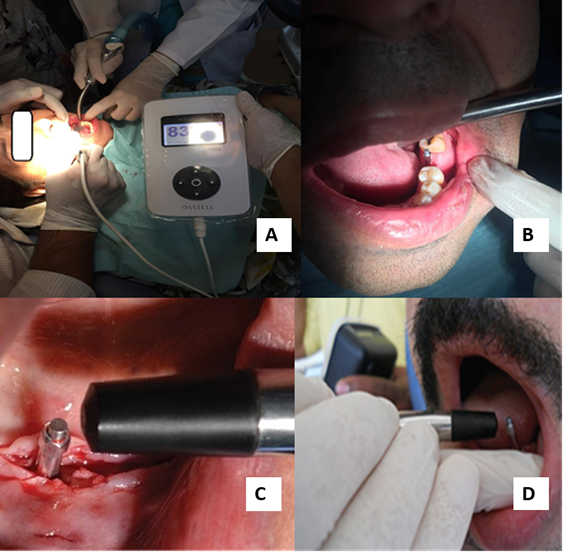
ISQ and OSI measurement through Ostelltm mentor device: The implant stability was measured following the protocol designed in a previous study (Youssef M, et al.,) (Figure 2A). 22 The Ostelltm device was initially calibrated using a test peg called the ISQ. A smart peg was used for assessment.
The smart peg tightened with 5 Ncm torque is then mounted on implant fixture and the transducer connected perpendicular to the implant (Figure 2B). The measuring probe is brought closer to the smart peg without touching it (Figure 2C and D). A beeping sound displays the reading on the monitor. Two successive readings are taken mesiodistally along the jaw and buccolingually perpendicular to the jaw (Figure 2). 23 The RFA measurements taken twice during implant treatment are recorded. All the ISQ values were recorded from one to hundred and means were taken.
Implant stability was calculated at the eight-month mark by the formula (ISQ2 – ISQ1 / healing time in months). Implant stability was measured on day zero in the start (ISQ1) and was remeasured at 8th week of implant stability (ISQ2) before functional loading. The categories of ISQ were defined as follows: ISQ < 60 depicts low stability, implants are at high risk of failure not suitable for loading; ISQ 60-65 depicts medium stability, where traditional loading or two-stage implant placement is recommended; ISQ 65-70 also depicts medium stability, a however single stage of loading or two-stage loading protocol can be considered, but ISQ > 70 shows high stability range, and so single stage loading protocol (immediate loading) may be considered. 24
Figure 2: Patient images of the digital readings shown on the Ostelltm mentor device on the chairside. (A) A cable used to attach probe to the instrument. (B) Smart peg screwed onto the implant fixture. (C) The measurement probe is brought closer to upper part of the smart peg (D). The probe was held in mesiodistal and buccolingual direction.
Figure 3: RFA values analysis through Ostelltm mentor (A) Diagrammatic illustration of the smart peg and (B) Measurements of RFA values were taken both in mesiodistal and buccolingual direction. Digital RFA values of 79 represented ISQ.
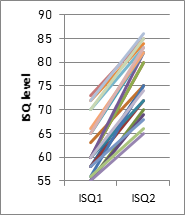
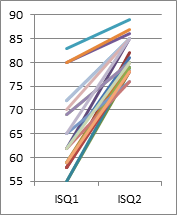
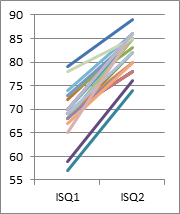
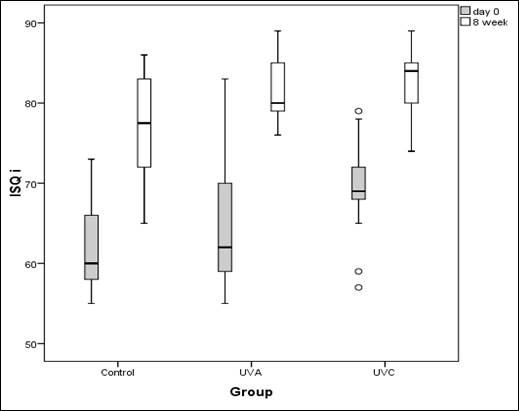
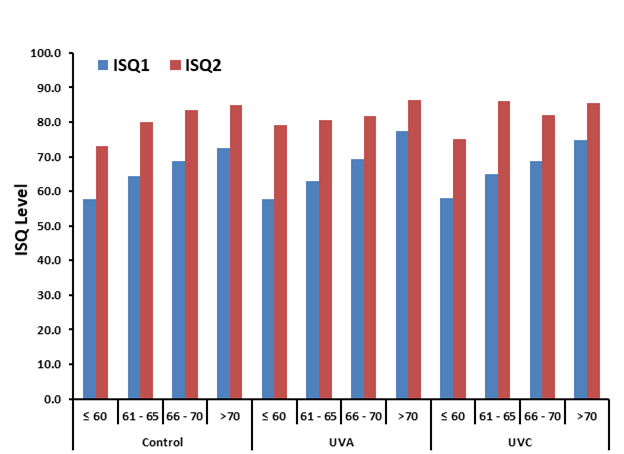
Statistical analysis for clinical trial: Statistical analysis was performed using SPSS version 26.0. Mean ± SD was used to represent ISQ levels and OSI data for each group. Line graphs illustrated variations between ISQ1 (baseline) and ISQ2 (8th-week values) for each treatment group, showing individual unit trends. Box plots were utilized to depict the distribution of ISQ1 and ISQ2 values across the three groups, while multiple bar diagrams demonstrated changes in ISQ relative to baseline values for each group.
Regression analysis was conducted to determine the effect of UVA and UVC irradiation on ISQ2, accounting for baseline ISQ values. A t-test was applied to compare the effects of UVA and UVC irradiation and assess statistical differences between the groups. Furthermore, a multiple linear regression model was employed to evaluate the impact of UVA and UVC treatments compared to the control group, while adjusting for baseline ISQ values.
A p-value of <0.05 was considered statistically significant for all analyses. This comprehensive approach ensured a robust evaluation of the treatment effects on implant stability and osseointegration.
RESULTS
Line graphs depicted that subject with low ISQ at baseline had more chances of progression, as visible in (Figure 3). The control group presented less than 65 ISQ at baseline, while in UVC, they mostly had ISQ over 65. There were numerous cases in the UVA group with baseline ISQ less than 60, 60-65, and more than 70.
The mean ISQ levels were 62.1 for the control group, while 65.2 for UVA and 69.3 for the UVC group (Table I). The difference at baseline between the three groups was found significant. The mean OSI (change in ISQ per month) was 7.4±1.7 for the control group, 8.5±3.3 for the UVA group, and 6.8±1.8 for the UVC group. The maximum gain was in the UVA group. The maximum increase in OSI was observed in UVA, followed by the control group and the UVC treated group (Table I), but baseline ISQ values were the highest for the UVC group. So, the mean ISQ levels in the 8th week were not directly comparable.
Table I: Mean ISQ levels at baseline and 8th week with OSI change per month
|
Groups |
Day 0 |
8th week |
Healing Time (OSI) |
|||
|
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
|
Control |
62.1 |
6.1 |
77.0 |
6.7 |
7.4 |
1.7 |
|
UVA |
65.2 |
8.2 |
81.5 |
3.7 |
8.5 |
3.3 |
|
UVC |
69.3 |
5.0 |
82.5 |
3.9 |
6.8 |
1.8 |
UVA: Ultraviolet A; UVC: Ultraviolet C; ISQ: implant stability quotient; OSI: Osseointegration speed index
|
Control |
UVA |
UVC |
Figure 4: Line graphs depicting the change between day 0 and the 8th week for individual subjects in each group.
The box plot also reflected the deployment of ISQ at baseline and 8th week time (Figure 4). The control group and UVA had close allocation at baseline. On the contrary, the UVC group had a varied and high median ISQ level at baseline compared to control and UVA, both after 8th weeks (Figure 4).
Figure 5: Box plot depicting ISQ values for each group at day 0 and 8th week.
A comparison was conducted irrespective of the group based on baseline ISQ levels. There were 23 subjects with ISQ < 60, which rose on average to 75. In 10 subjects with ISQ 61 to 65, the mean level improved to 81. It was seen that the subjects with lower ISQ at baseline had more improvement and the cases with higher ISQ levels at baseline had minor progress. This could also be followed within each group, i.e., lower the ISQ level at baseline and more probability of gain, as illustrated in the multiple bar diagram (Figure 5 and 6).
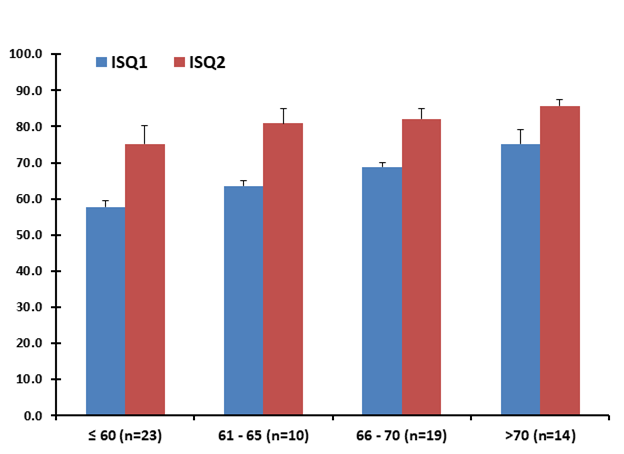
Figure 6: Multiple bar diagram showing the change in ISQ level concerning baseline status category, irrespective of the group.
Figure 7: Multiple bar diagram depicting a change in ISQ level concerning baseline status category, concerning the group by treatment.
A linear regression model was utilized to observe if the treatment affected the 8th week ISQ level, keeping in view the baseline values. In contrast, a t-test was applied to see the implication of the regression coefficient. The average ISQ level at the 8th week was 42.02 (significantly more than baseline) with a p-value < 0.001 (Table II). The influence of baseline value was also extremely significant with a p-value < 0.001 and triggered a change of 0.56 per 8th-week ISQ, maintaining treatments constantly. It was observed that the UVA had 2.83 units greater ISQ at the 8th week than control, holding the baseline consistent with a p-value of 0.009. The UVC group had no significant influence compared to the control and the p-value documented was 0.191 (Table II).
Table II: Multiple linear regression model showing effects of baseline ISQ values and groups on ISQ value at 8th week along with t-test
|
Coefficient Model |
Unstandardized Coefficients |
Standardized Coefficients |
t |
p-value |
|
|
B |
Std. Error |
Beta |
|||
|
(Constant) |
42.02 |
4.12 |
- |
10.20 |
<0.001* |
|
ISQ1 |
0.56 |
0.07 |
0.73 |
8.61 |
<0.001* |
|
UVA |
2.83 |
1.04 |
0.25 |
2.72 |
0.009* |
|
UVC |
1.49 |
1.12 |
0.13 |
1.32 |
0.191 |
a. Dependent Variable: ISQ2, B: Regression Coefficient; *p-value of <0.05 was considered statistically significant
DISCUSSION
The results of this study demonstrate that photofunctionalization of SLA-coated titanium implants with UVA irradiation significantly enhances implant stability and osseointegration compared to untreated implants, as evidenced by higher ISQ and OSI values at the 8th-week follow-up. UVA-treated implants exhibited a mean increase in ISQ by 8.5 ± 3.3 per month, surpassing both the control and UVC-treated groups. Although the UVC group showed higher baseline ISQ values, its impact on ISQ progression during the study period was less pronounced, and the difference compared to the control group was not statistically significant (p=0.191). These findings suggest that UVA irradiation may offer a more consistent and significant enhancement in implant stability, particularly for implants with lower baseline ISQ values, which showed greater improvement regardless of the treatment group. This highlights the potential of photofunctionalization as a promising intervention for optimizing implant success in areas of compromised bone quality.
Photofunctionalization has positive effect on implants ability to Osseointegrate with the bone. 7,25 UV irradiated implants promotes better healing then non-UV irradiated ones 16,26 and the implant stability is assessed clinically though ISQ values. 27
The implant stability was significantly more in the UVA group compared to control and UVC groups, respectively. Although both UVA and UVC were under strict observation, the results are in concordance with the previous literature showing UV irradiated implants with maximum increase in implant stability. 26
ISQ measurement varied among the three groups at initial stage showing individual variation. Direct comparison between ISQ values among the three groups cannot be made from baseline values. However, an increase in implant stability can be significantly appreciated at 8 weeks interval, even after applying the baseline values. The results are in accordance with a previous study suggesting increase in ISQ values at 12 weeks on SLA-coated implants although without photofunctionalization. 28 However, our study demonstrated an increase in ISQ values at eight weeks.
UVC implants irradiated before insertion showed lowest values at 8th week mark despite a higher baseline reading initially. A valid reason behind the increased baseline ISQ values in the UVC group (at the time of placement of implants) can be that the quality of the compact bone at the implant site might be much higher than the other two groups. Thus, resulting in initial higher ISQ values, as pointed out previously. 25
Keeping in view the changes seen at the baseline values, it was further noted that UVA irradiated implant fixtures depicted a maximum increase in ISQ values at the 8th week of treatment in comparison to the control and UVC irradiated groups. The theory behind the UVA group showing the highest rise in implant stability while UVC irradiated group depicting lower values can be explained by previous studies, which stated that Photofunctionalized implants significantly increased the ISQ and OSI values in all complicated cases. Photofunctionalization has no significant effect on implants with higher baseline initial values and stability. 12
We can deduce that the implants were placed in completely healed sockets with relatively good initial implant stability (initial ISQ values > 60 in all three groups). Hence, an increase in ISQ and OSI values over eight weeks in Photofunctionalized groups was not remarkable. It is emphasized that photofunctionalization is effective for implants with reduced primary stability, helping deal with complex cases. 12 Recent studies suggest using metformin to positively affect osseointegration in laboratory studies. 29 The effect of photodynamic therapy also showed promise in immediately loaded implants combined with scaling and root planning. 30
One limitation of this study was the relatively small sample size, as the project did not receive any assistance or funding from the government of Pakistan. Another significant challenge was the time constraint, which necessitated limiting the follow-up period to six months rather than the ideal duration of one year. Future studies are recommended to explore the long-term effects of UVA and UVC irradiation on peri-implant bone and implant stability, particularly in the context of immediate implant placement. Extending the follow-up period to one to five years would provide more comprehensive insights into the comparative efficacy and durability of these photofunctionalization.
CONCLUSIONS
This study demonstrated that UVA photofunctionalization significantly enhances implant stability and osseointegration in SLA-coated titanium implants, showing a strong correlation with improved ISQ and OSI values compared to untreated and UVC-treated implants. Baseline ISQ values played a key role in determining changes in ISQ, with UVA proving particularly effective in promoting treatment prognosis, especially in areas with compromised bone quality. These findings highlight the potential of UVA photofunctionalization as a reliable tool for improving dental implant outcomes. However, further research with larger sample sizes and extended follow-up periods is needed to validate these results and explore the long-term effects of UVA and UVC treatments.
ACKNOWLEDGMENT
We thank the Institute of Dentistry, CMH Lahore Medical College, and Universiti Sains Malaysia for offering procedural assistance on the Ostelltm mentor device.
REFERENCES
1. Amengual-Peñafiel L, Córdova LA, Jara-Sepúlveda CM, Brañes-Aroca M, Marchesani-Carrasco F, Cartes-Velásquez R. Osteoimmunology drives dental implant osseointegration: a new paradigm for implant dentistry. Jpn Dent Scie Rev 2021;57:12-9. https://doi.org/10.1016/j.jdsr.2021.01.001
2. Staedt H, Rossa M, Lehmann KM, Al-Nawas B, Kämmerer PW, Heimes D. Potential risk factors for early and late dental implant failure: a retrospective clinical study on 9080 implants. Int J Implant Dent 2020;6(1):81. https://doi.org/10.1186/s40729-020-00276
3. Al-Jamal MFJ, Al-Jumaily HA. Can the bone density estimated by cbct predict the primary stability of dental implants? a new measurement protocol. J Craniofac Surg 2021;32(2):e171-4. https://doi.org/10.1097/SCS.0000000000006991
4. Monje A, Ravidà A, Wang HL, Helms JA, Brunski JB. Relationship between primary/mechanical and secondary/biological implant stability. Int J Oral Maxillofac Implants 2019;34:s7-23. https://doi.org/10.11607/jomi.19suppl.g1
5. Andreotti AM, Goiato MC, Nobrega AS, da Silva EVF, Filho HG, Pellizzer EP, et al. Relationship between implant stability measurements obtained by two different devices: a systematic review. J Periodontol 2017;88(3):281-8. https://doi.org/10.1902/jop.2016.160436
6. Kaneko S, Yamamoto Y, Wada K, Kumagai G, Harada Y, Yamauchi R, et al. Ultraviolet irradiation improves the hydrophilicity and osteo-conduction of hydroxyapatite. J Orthop Surg Res 2020;15(1):1-8. https://doi.org/10.1186/s13018-020-01949-3
7. Yamauchi R, Itabashi T, Wada K, Tanaka T, Kumagai G, Ishibashi Y. Photofunctionalised Ti6Al4V implants enhance early phase osseointegration. Bone Joint Res 2017;6(5):331-6. https://doi.org/10.1302/2046-3758.65.BJR-2016-0221.R1
8. Aita H, Hori N, Takeuchi M, Suzuki T, Yamada M, Anpo M, et al. The effect of ultraviolet functionalization of titanium on integration with bone. Biomaterials 2009;30(6):1015-25. https://doi.org/10.1016/j.biomaterials.2008.11.004
9. Butera A, Gallo S, Pascadopoli M, Luraghi G, Scribante A. Ozonized water administration in peri-implant mucositis sites: a randomized clinical trial. Appl Sci 2021;11(17),7812. https://doi.org/10.3390/app11177812
10. Minamikawa H, Ikeda T, Att W, Hagiwara Y, Hirota M, Tabuchi M, et al. Photofunctionalization increases the bioactivity and osteoconductivity of the titanium alloy Ti6Al4V. J Biomed Mater Res A 2014;102(10):3618-30. https://doi.org/10.1002/jbm.a.35030
11.
Flanagan D. Photofunctionalization of dental implants. J Oral Implantol
2016;42(5):445-50.https://doi.org/10.1563/aaid-joi-D-15-00145
12. Hirota M, Ozawa T, Iwai T, Ogawa T, Tohnai I. Implant stability development of photofunctionalized implants placed in regular and complex cases: a case-control study. Int J Oral Maxillofac Implants 2016;31(3):676-86. https://doi.org/10.11607/jomi.4115
13. Funato A, Ogawa T. Photofunctionalized dental implants: a case series in compromised bone. Int J Oral Maxillofac Implants 2013;28(6):1589-601. https://doi.org/10.11607/jomi.3232
14. Zaheer N, Bin Rajion ZA, Maliha S, Hariy P, Muhammad QS, Noor HAR. Ultraviolet A and Ultraviolet C light-induced reduction of surface hydrocarbons on titanium implants. Eur J Dent 2019;13(1):114-8. https://doi.org/10.1055/s-0039-1688741
15. Zaheer N, Abdullah AM, Rajion ZA, Shahbaz M, Zaheer U, Saeed MQ, et al. Ultraviolet A and ultraviolet C light-induced effect on titanium implant surface. Acta Microscopica 2021;30(2):41-8.
16. Suzuki S, Kobayashi H, Ogawa T. Implant stability change and osseointegration speed of immediately loaded photofunctionalized implants. Implant Dent 2013;22(5):481-90. https://doi.org/10.1097/id.0b013e31829deb62
17. Zaheer N, Bin Rajion ZA, Shahbaz M, Zaheer U, Saeed MQ, Abdul Razak NH. Bone density and marginal bone loss around implants post ultraviolet A and ultraviolet C irradiation. Sains Malays 2020;49(6):1411-20. http://dx.doi.org/10.17576/jsm-2020-4906-19
18. Hirota M, Ozawa T, Iwai T, Ogawa T, Tohnai I. Effect of photofunctionalization on early implant failure. Int J Oral Maxillofac Implants 2018;33(5):1098-102. https://doi.org/10.11607/jomi.6541
19. Funato A, Tonotsuka R, Murabe H, Hirota M, Ogawa T. A novel strategy for bone integration and regeneration: case studies. J Cosmetic Dent 2014;29(4):74-86.
20. Cohen J. Statistical power analysis for the behavioral sciences. Statistical Power Analysis for the Behavioral Sciences. Routledge; 2013. https://doi.org/10.4324/9780203771587
21. Kitajima H, Ogawa T. The Use of Photofunctionalized Implants for Low or Extremely Low Primary Stability Cases. Int J Oral Maxillofac Implants 2016;31(2):439-47. https://doi.org/10.11607/jomi.4054
22. Youssef M, Shaaban AM, Eldibany R. The correlation between bone density and implant stability. Alex Dent J 2015;40:15-21.
23. Genisa M, Rajion ZA, Shuib S, Pohchi A, Mohamad D. Behavior of implant stability during implant treatment: in vivo study. J Teknol 2015;76(7):51-5. http://dx.doi.org/10.11113/jt.v76.5714
24. Trisi P, Carlesi T, Colagiovanni M, Perfetti G. Implant stability quotient (ISQ) vs direct in vitro measurement of primary stability (micromotion): effect of bone density and insertion torque. J Osteol Biomat 2010;1(3):141-9.
25. Mehl C, Kern M, Neumann F, Bähr T, Wiltfang J, Gassling V. Effect of ultraviolet photofunctionalization of dental titanium implants on osseointegration. J Zhejiang Univ Sci B 2018;19(7):525-34. https://doi.org/10.1631/jzus.b1600505
26. Funato A, Yamada M, Ogawa T. Success rate, healing time, and implant stability of photofunctionalized dental implants. Int J Oral Maxillofac Implants. 2013;28(5):1261-71. https://doi.org/10.11607/jomi.3263
27. Chan HL, El-Kholy K, Fu JH, Galindo-Moreno P, Wang HL. Implant primary stability determined by resonance frequency analysis in surgically created defects: a pilot cadaver study. Implant Dent 2010;19(6):509-19. https://doi.org/10.1097/id.0b013e3181fa7f6a
28. Huwiler MA, Pjetursson BE, Bosshardt DD, Salvi GE, Lang NP. Resonance frequency analysis in relation to jawbone characteristics and during early healing of implant installation. Clin Oral Implants Res 2007;18(3):275-80. https://doi.org/10.1111/j.1600-0501.2007.01336.x
29. Yıldırım TT, Dündar S, Bozoğlan A, Karaman T, Kahraman OE, Özcan EC. The effects of metformin on the bone filling ration around of TiAl6Va4 implants in non diabetic rats. J Oral Biol Craniofac Res 2020;10(4):474-7. https://doi.org/10.1016/j.jobcr.2020.07.012
30. Vardhan PK, Paramashivaiah R, Prabhuji MLV, Bhavikatti SK, Basha S, Arora S, et al. The effect of photodynamic therapy on the early outcome of implants placed on patients with periodontitis. Photonics 2022;9(7):480. https://www.mdpi.com/2304-6732/9/7/480#
AUTHORS' CONTRIBUTIONS Following authors have made substantial contributions to the manuscript as under: NZ, UZ & ZABR: Conception and study design, acquisition of data, drafting the manuscript, approval of the final version to be published MS: Acquisition of data, drafting the manuscript, approval of the final version to be published AMZ & MQS: Analysis and interpretation of data, approval of the final version to be published
Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work.
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |