![]() https://doi.org/10.35845/kmuj.2024.23536 ORIGINAL ARTICLE
https://doi.org/10.35845/kmuj.2024.23536 ORIGINAL ARTICLE
Comparison of spinal stabilization exercise versus Maitland
mobilization along with laser therapy in non-specific low back pain
Khizra Ashraf ![]() 1,
2, Areeba Tauseef
1,
2, Areeba Tauseef ![]() 1,3,
Zarafshan Sajid
1,3,
Zarafshan Sajid ![]() 1
, Wajeeha Mahmood
1
, Wajeeha Mahmood ![]() 1,4,
Tahir Mahmood
1,4,
Tahir Mahmood ![]() 5,
Muhammad Naveed Babur
5,
Muhammad Naveed Babur ![]() 1
1
|
1: Department of Physiotherapy, Faculty of Rehabilitation and Allied Health Sciences, Choudhary Muhammad Akram Research and Teaching Hospital, Superior University, Lahore, Pakistan 2: Department of Physiotherapy, Government Services Hospital, Lahore, Pakistan 3: Department of Physiotherapy, Salman Hospital, Lahore, Pakistan 4: Department of Physical Therapy, University of Health Sciences, Lahore, Pakistan 5: Department of Physical Therapy, Rashid Latif Khan University, Lahore, Pakistan
Email Contact #: +92-300- 6741320
Date Submitted: November 17, 2023 Date Revised: August 03, 2024 Date Accepted: August 21, 2024 |
|
THIS ARTICLE MAY BE CITED AS: Ashraf K, Tauseef A, Sajid Z, Mahmood W, Mahmood T, Babur MN. Comparison of spinal stabilization exercise versus Maitland mobilization along with laser therapy in non-specific low back pain. Khyber Med Univ J 2024;16(3):195-200. https://doi.org/10.35845/kmuj.2024.23536 |
ABSTRACT
OBJECTIVE:
To compare the effects of spinal stabilization exercises versus Maitland
mobilization and laser therapy on non-specific low back pain (NSLBP).
METHODS: This randomized controlled trial was conducted at Al-Noor Physio Center, Tayyab Physiotherapy Clinic, and Al-Zahra Medical Complex between June and December 2022. Study included 50 patients aged 18-60 years with NSLBP, selected through a simple random sampling technique. Participants were randomly assigned to Group-A (spinal stabilization and laser therapy) and Group-B (Maitland mobilization and laser therapy). Both groups received interventions three times a week for eight weeks. The primary outcomes-pain, disability, and lumbar range of motion (ROM)-were assessed using pre- and post-intervention tests with appropriate statistical analyses.
RESULTS: Of the 50 participants, 28 (56%) were male and 22 (44%) female, with a mean age of 45.66 ± 8.48 years in Group-A and 44.68 ± 9.42 years in Group-B. Both groups were comparable at baseline in terms of age (p =0.10) and gender (p>0.05). The within-group analysis revealed significant reductions in pain, disability, and ROM in both groups (p <0.05). Group A showed a median pain score of 3.0 (IQR 2.0-3.0) compared to 5.0 (IQR 4.50-6.0) in Group-B, and a median disability score of 7.0 (IQR 7.0-8.0) compared to 14.0 (IQR 12.0-15.0) in Group-B (p <0.05). ROM improvements included lumbar flexion (p=0.02), hyperextension (p = 0.00), and side flexion (p=0.00), with Group-A outperforming Group-B.
CONCLUSION: Spinal stabilization exercises were more effective than Maitland mobilization in reducing pain, improving disability, and enhancing lumbar ROM in patients with NSLBP.
Clinical Trial Registration Number: NCT05421871
KEY WORDS: Disability (MeSH); Disability Evaluation (MeSH); Insurance, Disability (MeSH); Intellectual Disability (MeSH); Laser therapy (Non-MeSH); Low Back Pain (MeSH); Maitland Mobilization (MeSH); Quality Of Life (MeSH); Stabilization exercise (Non-MeSH); Trunk mobility (Non-MeSH).
INTRODUCTION
Nonspecific low back pain (LBP) refers to back pain not caused by any identifiable pathology, disease, or deformity and can be classified as acute, sub-acute, or chronic, based on its duration.1 The prevalence of LBP among female students is 43.3%, while it is 20% among homemakers.2 In Pakistan, 56.25% of the population experiences LBP, with 58.8% reporting job-related difficulties. Risk factors for nonspecific LBP are categorized into psychological, physiological, and physical factors. Physical factors include activities such as weightlifting, prolonged standing, heavy manual labor, long periods of sitting, and poor posture in computer workers.3 If left untreated, nonspecific LBP in young adults can lead to conditions like nonstructural scoliosis.4
LBP affects people globally, with higher risk among those with physically demanding jobs, physical and mental health issues, or obesity.5 The incidence of chronic LBP increases from the third decade of life to age 60, with women being more frequently affected.6 Chronic LBP treatment approaches are categorized by invasiveness: non-invasive without medication, non-invasive with medication, and invasive treatments like surgery or injections.7 Guidelines recommend managing LBP through physical activity, physiotherapy, and medications.8 Systematic reviews have demonstrated that stabilization exercises effectively reduce pain and disability in nonspecific LBP,9 improving core stability and muscular endurance.10
Low-level laser therapy (LLLT) has gained popularity in treating musculoskeletal, neurological, and rheumatologic conditions.11 LLLT influences the inflammatory, proliferative, and remodeling phases of healing and provides analgesia by inhibiting pain-producing neurons. Maitland manual therapy, combined with core stabilization exercises, has been shown to improve chronic LBP more effectively than standard physical therapy.12 Techniques like sustained natural apophyseal glides enhance postural stability and alleviate pain, even when flexion is dominant.13 As nonspecific LBP is a leading cause of disability, it presents a significant social burden that must be addressed.14 This study was planned to evaluate the effects of spinal stabilization exercises versus Maitland mobilization and laser therapy in managing nonspecific LBP, providing valuable insights for clinicians on conservative treatment options for low back pain.
METHODS
This randomized controlled trial was conducted following ethical approval (Ref# FAHS/DPT/1/23/A-13587) and prospectively registered under registration #NCT05421871. The trial was conducted from June 20, 2022, to December 2022, with data collected from Al Noor Physio Center, Ferozepur Road, Tayyab Physiotherapy Clinic, and Al Zahra Medical Complex Lahore, Pakistan. Fifty participants who met the inclusion criteria were recruited and randomly assigned to Group A or Group B using the lottery method. The calculated sample size was 52, accounting for a 10% drop-out rate, and was determined using the Visual Analogue Scale (VAS) as the outcome measurement. The formula used for sample size calculation was n = [(z α/2+ zβ)² (µ1-µ2)²], where n represents the sample size per group, z α/2 is 1.96 for a 5% significance level, and zβ is 0.84 for 80% power. The standard deviation (σ) was 1.65, µ1 (change in mean VAS score in the experimental group) was 3.05, and µ2 (change in mean VAS score in the control group) was 4.39. ¹¹
The inclusion criteria involved diagnosed cases of non-radiating low back pain in males and females aged 18-60 years15 with a pain score of >3. Patients with spinal injuries, spinal stenosis, degenerative changes, neuropathy, intervertebral disc collapse, discectomy, or laminectomy were excluded. 16 The data was collected using a simple random sampling technique. Ethical standards, including confidentiality and participant identity protection, were strictly followed in line with the Helsinki Declaration. After obtaining all necessary permissions from the administration, participants signed informed consent forms. The study adhered to CONSORT guidelines, and all patients were screened accordingly. The allocation process was concealed and carried out by a research assistant uninvolved in any further research steps. The assistant was only aware of the outcome evaluation, not the intervention allocation, and handed the completed data over to the investigators.
Prior to collecting baseline readings, a thorough screening of patient history was conducted to identify any pathology leading to low back pain, injuries, and to ensure adherence to the study's exclusion criteria. Baseline outcome data were gathered using the Visual Analogue Scale (VAS), which ranges from 0-10, with 0 indicating mild pain and 10 representing severe pain. The validity of VAS ranges from 0.16 to 0.51.¹⁸ The Roland-Morris Disability Questionnaire was employed to assess changes in physical disability among low back pain patients. This questionnaire consists of 24 questions, and the number of items marked by the patient determines the score. If a patient indicates that a question does not apply, it is scored as No or 0. A score of 0 represents no disability, whereas scores of 11, 18, or 24 indicate increasing levels of disability. The higher the score, the greater the disability, and the questionnaire has a reliability of 0.91. ¹⁹
A goniometer was used to measure any increase in the range of motion (ROM). For lumbar hyperextension, the landmarks for goniometer alignment included the fulcrum placed at the junction of the anterior superior iliac supine, the immobile arm aligned along the pelvis midline, and the measuring arm aligned with the mid-axillary line. For lateral flexion, the alignment landmarks involved the stationary arm positioned on the spinous process of the L-5 vertebrae, with the fulcrum on the mid-back, and the measuring arm aligned with the C-7 vertebrae spinous process. For lumbar flexion, the stationary arm bisected the anterior superior iliac supine, the fulcrum was placed on the iliac crest, and the measuring arm bisected the mid-axillary line. The reliability of the goniometer as a measuring tool is considered good to excellent, ²⁰ with a validity of ≥ 0.85. ²¹ All outcomes were measured by a blinded assessor, and the measurements were taken at baseline and after eight weeks of intervention.
All participants were assured of the privacy and confidentiality of their data. The researcher strictly adhered to ethical guidelines throughout the study, ensuring no violations occurred. Participants were informed of their right to withdraw from the study at any time. Descriptive statistics were used to summarize qualitative data, and frequencies were calculated for categorical variables. Data analysis was conducted using SPSS version 23. The normality of the data was assessed using the Kolmogorov-Smirnov and Shapiro-Wilk tests. Pain and disability within groups were analyzed using the Wilcoxon signed-rank test, with results presented as median and interquartile range (IQR), while between-group differences were assessed using the Mann-Whitney U test. For within-group comparisons of ROM, presented as Mean ± SD (based on normal distribution, Shapiro-Wilk test p >0.05), the paired t-test was applied. Between-group comparisons were conducted using the independent sample t-test. A p-value of ≤0.05 was considered statistically significant.
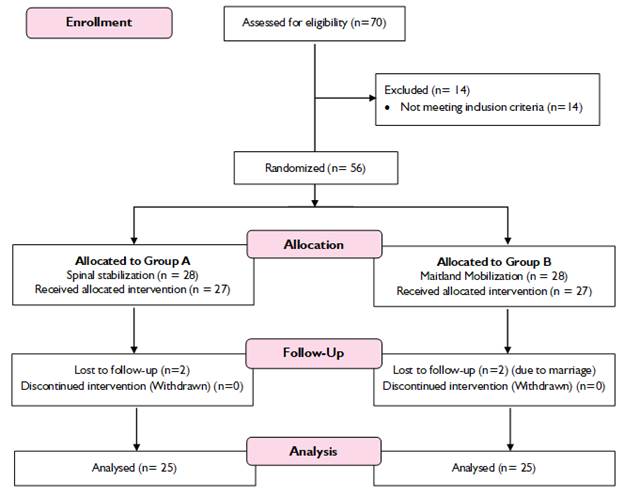
Figure 1: CONSORT Flow chart showing enrollment, intervention allocation, and follow-up
RESULTS
Out of the 50 participants, 25 were assigned to the stabilization treatment group, consisting of 12 males and 13 females, while the remaining 25 were enrolled in the Maitland mobilization treatment group, which included 16 males and 9 females. The mean age of participants in the spinal stabilization Group (A) was 45.66 ± 8.48 years, and in the Maitland mobilization Group (B), it was 44.68 ± 9.42 years. Both groups were comparable at baseline in terms of age and gender, with no statistically significant differences (p-value = 0.10 for age and >0.05 for gender) among those with chronic non-specific LBP (Table I).
Table I: Sociodemographic profile of the study participants
|
Variables |
Category |
Spinal Stabilization Group A (n=25) |
Maitland Group B (n=25) |
p-value |
|
Gender |
Male |
12 |
16 |
1.00 |
|
Female |
13 |
9 |
0.06 |
|
|
Age (years) |
Mean ±SD |
45.66±8.48 |
44.68±9.42 |
0.10 |
The within-group analysis revealed a significant reduction in pain in Group A compared to Group B, with a p-value of <0.05. In Group A, pre- and post-test comparisons showed significant improvements in lumbar flexion, extension, as well as left and right lateral flexion (p = 0.00), which were more pronounced than those observed in Group B (p < 0.05). Similarly, the Disability Index, presented as Median (IQR), indicated a reduction in disability in both groups (p < 0.05) (Table II).
Table II: Within-group comparison of pain, disability, and range of motion
|
Outcomes |
Evaluation |
Spinal Stabilization Group A (n=25) |
Maitland Group B (n=25) |
||
|
Median (IQR) |
p-value |
Median (IQR) |
p-value |
||
|
Pain |
Pre-Test Pain |
8.0 (8.0-9.00) |
0.00 |
9.0 (8.0-9.0) |
0.00 |
|
Post-Test Pain |
3.0( 2.0-3.0) |
5.0 (4.50-6.0) |
|||
|
Disability |
Pre-test Disability |
17.0( 16.0-18.50) |
0.01 |
18.0 (17.0-19.0) |
0.00 |
|
Post-test Disability |
7.0(7.0-8.0) |
14.0 (12.0-15.0) |
|||
|
|
Mean± SD |
|
Mean± SD |
|
|
|
Range of Motion (Degrees) |
Pretest Lumber Flexion |
38.64±2.91 |
0.00 |
38.52±3.39 |
0.00 |
|
Posttest Lumber Flexion |
49.56±2.72 |
47.32±3.87 |
|||
|
Pretest Lumber Hyperextension |
13.12±1.36 |
0.00 |
12.92±1.18 |
0.00 |
|
|
Posttest Lumber Hyperextension |
19.72±1.990 |
17.96±2.30 |
|||
|
Pretest Lumber Side Flexion Left |
12.68±1.145 |
0.00 |
12.36±1.28 |
0.00 |
|
|
Posttest Lumber Side Flexion Left |
20.20±1.803 |
18.64±2.07 |
|||
|
Pretest Lumber Side Flexion Right |
12.64±1.41 |
0.00 |
12.24±1.45 |
0.00 |
|
|
Posttest Lumber Side Flexion Right |
20.32±1.28 |
18.76±1.85 |
|||
Pain and ODI=IQR: Inter Quartile Range, Wilcoxon Signed Ranks, ROM is analyzed using Paired t-test, *p-value ≤ 0.05
Between groups A and B analysis, the pretest and posttest showed significant differences in pain and disability, ROM, and disability index. (P-value<0.05). Group A showed statistically significant improvements compared to Group B (Table No. III)
Table III: Between-group differences in pain, disability, and range of motion
|
Outcomes |
Evaluation |
Spinal Stabilization Group A (n=25) |
Maitland Group B (n=25) |
p-value |
|
Median (IQR) |
Median (IQR) |
|||
|
Pain |
Pretest posttest Pain |
3.0( 2.0-3.0) |
5.0 (4.50-6.0) |
0.02 |
|
Disability |
Pretest Posttest Disability |
7.0(7.0-8.0) |
14.0 (12.0-15.0) |
0.00 |
|
|
Mean ±SD |
Mean ±SD |
|
|
|
Range of Motion (Degrees) |
Pretest Posttest Lumber Flexion |
-10.92±225 |
-8.8±3.02 |
0.02 |
|
Pretest Posttest Lumber Hyper extension |
-6.6±1.63 |
-5.04±2.26 |
0.00 |
|
|
Pretest Posttest left side Lumber Flexion |
-7.52±1.55 |
-6.28±2.03 |
0.00 |
|
|
Pretest Posttest Right Lumber Side Flexion |
-7.68±1.03 |
6.52±2.14 |
0.00 |
|
Pain and ODI, =IQR: Inter Quartile Range, Mann–Whitney U test applied, ROM is analyzed using independent sample t-test, *p-value ≤ 0.05
DISCUSSION
The findings of this study, which compared the effects of spinal stabilization exercises with Maitland mobilization and laser therapy in managing non-specific low back pain in 52 patients, indicate that spinal stabilization exercises are more effective in reducing pain, improving disability, and enhancing ROM (p = 0.00). Similar findings have been observed in previous studies, such as one demonstrating that lumbar spine stabilization exercises combined with laser therapy significantly enhanced ROM and strength, particularly in extension, rotation, and flexion, compared to laser therapy and kinesio-taping alone. ³ The current study demonstrated a statistically significant reduction in pain, disability, and ROM in both Group A and Group B (p-value < 0.05). This can be attributed to the combined effects of lumbar stabilization and walking exercises, which significantly enhanced mobility. Stabilization exercises notably increased the muscular endurance of the back muscles and improved core stability. ¹⁰ Additionally, stabilization exercises have proven to be more effective than conventional physical therapy exercises in reducing pain in patients with lower back pain. ²²
The study also highlights that pain, disability, and ROM can be further improved through spinal exercises in combination with laser therapy. Another study supports this by demonstrating that the combination of stabilization exercises and laser therapy is effective in reducing pain, improving disability, and enhancing ROM.²³ Additionally, spinal and trunk exercises have proven effective in managing non-specific LBP, although a study focusing on females only was limited in its scope.²⁴ When examining the combined effects of the Maitland technique, spinal stabilization, and lumbar traction on ROM, pain, and disability in patients with chronic back pain, it is evident that combination interventions yield better results than individual techniques.²⁵ However, no single technique showed the same effectiveness as combination therapy, with the Maitland group demonstrating comparatively lesser improvements.
The current study suggests that a structured intervention program, along with accurate patient education, could transform the management of chronic back pain. Another study found that stabilization exercises led to significant improvements in pain and functional disability after 12 sessions over 4 weeks when compared to a control group.²⁶ Manual therapy has emerged as a potential alternative for treating LBP, but adherence to the treatment regimen, patient expectations, and factors such as cost and recovery time can impact its effectiveness.²⁷ Moreover, the combined use of Mulligan mobilization and low-level laser therapy has been found to be an effective approach for reducing pain and increasing ROM and functional levels in patients with chronic LBP.¹¹
Similarly, when comparing the outcomes to pilates exercises combined with kinesiotaping for LBP, as reported in a local study,²⁸ the findings of the current study are consistent, demonstrating similar effectiveness for managing LBP. Gopal Nambi also concluded that spinal manipulation combined with laser therapy and conventional therapy is more effective than conventional exercises and laser therapy alone for chronic low back pain patients.²⁹
It can be stated that conservative interventions should be prioritized in managing pain to enhance patients' daily functioning and reduce their dependency. The outcomes of this study support the use of such interventions as an effective regimen for managing non-specific LBP. However, despite the advantages, some female participants were hesitant to receive laser therapy. Moreover, the small sample size limits the ability to detect significant differences, and the study's short duration only allowed for the assessment of short-term effects.
Future studies should also consider evaluating patients' lifestyles and occupational factors to enhance the accuracy and relevance of research outcomes. Additionally, educational seminars aimed at raising awareness about the benefits of laser therapy, particularly for female patients, could help address concerns and improve the acceptance of this treatment method.
CONCLUSION
This study concludes that spinal stabilization exercises are more effective than Maitland mobilization in reducing pain, improving disability, and enhancing lumbar mobility (lumbar flexion) in patients with non-specific low back pain. These protocols can be employed to improve pain management, range of motion, and disability indices, thereby potentially enhancing the quality of life and reducing the risk of disability in the target population.
REFERENCES
1. Cashin AG, Folly T, Bagg MK, Wewege MA, Jones MD, Ferraro MC, et al. Efficacy, acceptability, and safety of muscle relaxants for adults with non-specific low back pain: systematic review and meta-analysis. Br Med J 2021;374:n1446. https://doi.org/10.1136/bmj.n1446
2. Sadia H, Munawar A, Tanveer F, Ahmed A, Gilani SA. Frequency of low back and neck pain among female drivers. Rawal Med J 2019;44(2):365-7.
3. Kotagiri S, Mathur N, Kumar A, Song AK. Effectiveness of lumbar stabilization exercises with laser therapy in patients with mechanical low back pain. Int Arch Integr Med 2019;6(9):117-26.
4. Khubaib F, Maqsood U, Mahmood T, Arshad HS, Mahmood W. Risk factors of non-structural scoliosis in adults with low back pain. Rawal Med J 2019;44(3):498-501.
5. Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet 2018;391(10137):2356-67. https://doi.org/10.1016/s0140-6736(18)30480-x
6. Meucci RD, Fassa AG, Faria NMX. Prevalence of chronic low back pain: systematic review. Rev Saude Publica. 2015;49:1. https://doi.org/10.1590/s0034-8910.2015049005874
7. Ogundiran O, Ogunsanya G. The Relative Efficacy of a six-week tripartite physiotherapeutic modality in the management of chronic low back pain. Int J Advanced Res Pub 2017;1(4):243-5.
8. George SZ, Fritz JM, Silfies SP, Schneider MJ, Beneciuk JM, Lentz TA, et al. Interventions for the management of acute and chronic low back pain: revision 2021. J Orthop Sports Phys Ther 2021;51(11):CPG1-CPG60. https://doi.org/10.2519/jospt.2021.0304
9. Mueller J, Niederer D. Dose-response-relationship of stabilisation exercises in patients with chronic non-specific low back pain: a systematic review with meta-regression. Sci Rep 2020;10(1):16921. https://doi.org/10.1038/s41598-020-73954-9
10. Suh JH, Kim H, Jung GP, Ko JY, Ryu JS. The effect of lumbar stabilization and walking exercises on chronic low back pain: a randomized controlled trial. Medicine (Baltimore) 2019;98(26):e16173. https://doi.org/10.1097/md.0000000000016173
11. Seo U-H, Kim J-H, Lee B-H. Effects of Mulligan mobilization and low-level laser therapy on physical disability, pain, and range of motion in patients with chronic low back pain: a pilot randomized controlled trial. Healthcare (Basel) 2020;8(3):237. https://doi.org/10.3390/healthcare8030237
12. Ahmed F, Rahman MU, Ullah K, Bhutta AH. Combination of core stability exercises and maitland manual therapy is better alternative in the management of chronic low back pain. J Riphah Coll Rehabil Sci 2020;8(1):S24-S8. https://doi.org/10.5455/JRCRS. 202008SI06
13. Hussein HM, Morsi AA, Abdelraoof NA. The immediate effect of sustained natural apophyseal glide on postural stability and pain in individuals presenting with flexion-dominant chronic low back pain: a randomized single-blinded placebo-controlled trial. J Back Musculoskelet Rehabil 2021;34(6):1079-86. https://doi.org/10.3233/bmr-200217
14. Dal Farra F, Risio RG, Vismara L, Bergna A. Effectiveness of osteopathic interventions in chronic non-specific low back pain: a systematic review and meta-analysis. Complement Ther Med 2021;56:102616. https://doi.org/10.1016/j.ctim.2020.102616
15. Hradetzky E, Ohlmeier C, Brinkmann C, Schild M, Galetzka W, Schmedt N, et al. Epidemiology and routine care treatment of patients with hip or knee osteoarthritis and chronic lower back pain: real-world evidence from Germany. J Pub Health 2022;30(12):2855-67. https://doi.org/10.1007/s10389-022-01700-8
16. Javaherian M, Tajali SB, Moghaddam BA, Keshtkar AA, Azizi M. Immediate effects of Maitland mobilization and Mulligan techniques on flexion and extension range of motion in patients with chronic nonspecific low back pain: a randomized pilot study. J Mod Rehabil 2017;11(2):127-32.
17. Glazov G, Yelland M, Emery J. Low-dose laser acupuncture for non-specific chronic low back pain: a double-blind randomised controlled trial. Acupunct Med 2014;32(2):116-23. https://doi.org/10.1136/acupmed-2013-010456
18. Boonstra AM, Preuper HRS, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 2008;31(2):165-9. https://doi.org/10.1097/mrr.0b013e3282fc0f93
19. Brouwer S, Kuijer W, Dijkstra PU, Göeken LN, Groothoff JW, Geertzen JH. Reliability and stability of the Roland Morris Disability Questionnaire: intra class correlation and limits of agreement. Disabil Rehabil 2004;26(3):162-5. https://doi.org/10.1080/09638280310001639713
20. De Carvalho RMF, Mazzer N, Barbieri CH. Analysis of the reliability and reproducibility of goniometry compared to hand photogrammetry. Acta Ortop Bras 2012;20(3):139-49. https://doi.org/10.1590/s1413-78522012000300003
21. Alamrani S, Rushton AB, Gardner A, Bini E, Falla D, Heneghan NR. Physical functioning in adolescents with idiopathic scoliosis: a systematic review of outcome measures and their measurement properties. Spine (Phila Pa 1976) 2021;46(18):E985-E97. https://doi.org/10.1097/brs.0000000000003969
22. Akhtar MW, Karimi H, Gilani SA. Effectiveness of core stabilization exercises and routine exercise therapy in management of pain in chronic non-specific low back pain: a randomized controlled clinical trial. Pak J Med Sci 2017;33(4):1002-6. https://doi.org/10.12669/pjms.334.12664
23. Alami S, Nakhostin-Roohi B. The effect of core stabilization exercise (CSE) and high-power laser (HPL) on chronic low back pain (CLBP) in female athletes. New Approaches Exerc Physiol 2022;4(8):71-88. https://doi.org/10.22054/nass.2023.70017.1120
24. Minobes-Molina E, Nogués MR, Giralt M, Casajuana C, de Souza DLB, Jerez-Roig J, et al. Effectiveness of specific stabilization exercise compared with traditional trunk exercise in women with non-specific low back pain: a pilot randomized controlled trial. PeerJ 2020;8:e10304. https://doi.org/10.7717/peerj.10304
25. Mohamed HE, Elsayed WH, Aneis YM. The combined effect of Maitland spinal mobilization with mechanical lumbar traction in patients with chronic nonspecific low back pain. Egypt J Appl Sci 2020;35(12):136-50. https://doi.org/10.21608/ejas.2020.142520
26. Batool F, Afzal W, Ahmad A, Gilani SA. Effectiveness of core stability with and without neck extension on pain intensity and functional disability in patients with chronic low back pain. Rawal Med J 2019;44(4):797-800.
27. Phelan A, Phelan K, Foley M. Effectiveness of maitland spinal mobilisation therapy in the treatment of non-specific low back pain–a prospective study of clients attending a single treatment centre in the Republic of Ireland. Phys Ther Rehabil 2020;7(1):7. http://dx.doi.org/10.7243/2055-2386-7-7
28. Akram A, Imtiaz K, Maryem S, Mahmood W, Mahmood T, Babur MN. Comparison of Pilates exercises versus muscle energy technique with Kinesio taping in non-specific low back pain: a randomized controlled trial. Khyber Med Univ J 2024;16(1):3-9. https://doi.org/10.35845/kmuj.2024.23415
29. Nambi G, Kamal W, Es S, Joshi S, Trivedi P. Spinal manipulation plus laser therapy versus laser therapy alone in the treatment of chronic non-specific low back pain: a randomized controlled study. Eur J Phys Rehabil Med 2018;54(6):880-9. https://doi.org/10.23736/s1973-9087.18.05005-0
Following authors have made substantial contributions to the manuscript as under:
KA: Study design, acquisition of data, drafting the manuscript, approval of the final version to be published AT: Acquisition of data, drafting the manuscript, approval of the final version to be published ZS: Analysis and interpretation of data, critical review, approval of the final version to be published WM: Conception and study design, critical review, approval of the final version to be published TM & MNB: Acquisition of data, drafting the manuscript, approval of the final version to be published
Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work.
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |