![]() https://doi.org/10.35845/kmuj.2023.23442
ORIGINAL
ARTICLE
https://doi.org/10.35845/kmuj.2023.23442
ORIGINAL
ARTICLE
Association of recurrent A1090E variant of OTOFERLIN (OTOF) gene with non-syndromic hereditary sensorineural hearing loss in Pakistani population
Isma Riaz1,2![]() ,
Amir Rashid2, Asifa Majeed2, Kashif Obaid Khan Niazi2,
Hammad Gul Khan3
,
Amir Rashid2, Asifa Majeed2, Kashif Obaid Khan Niazi2,
Hammad Gul Khan3
|
1: Department of Biochemistry, Rawalpindi Medical University, Rawalpindi, Pakistan. 2:Department of Biochemistry and Molecular Biology, Army Medical College, National University of Medical Sciences, Rawalpindi, Pakistan. 3: Department of ENT, Combined Military Hospital Rawalpindi, Pakistan
Email
Contact #: +92-301-5555622
Date Submitted: August10, 2023 Date Revised: October 22, 2023 Date Accepted: November10, 2023 |
|
THIS ARTICLE MAY BE CITED AS: Riaz I, Rashid A, Majeed A, Niazi KOK, Khan HG. Association of recurrent A1090E variant of OTOFERLIN (OTOF) gene with non-syndromic hereditary hearing loss in Pakistani population. Khyber Med Univ J 2023;15(4):218-22. https://doi.org/10.35845/kmuj.2023.23442 |
ABSTRACT
OBJECTIVES: To detect the presence of the otoferlin A1090E variant and investigate its potential correlation with severe to profound non-syndromic hereditary sensorineural hearing loss (NSHSHL) in Pakistani cochlear implant recipients.
METHODS: This case-control study, conducted from January to December 2022, comprised 100 cases of age 6 months to 10 years of severe to profound NSHSHL who had undergone cochlear implant at ENT Department CMH Rawalpindi, and 100 healthy age matched individuals recruited from CMH Rawalpindi. Blood samples underwent DNA extraction, polymerase chain reaction, and subsequent restriction fragment length polymorphism (RFLP) analysis at the Center for Research in Experimental and Applied Medicine, Army Medical College, Rawalpindi. Statistical analysis was done through SPSS, and genetic analysis employed SNP Stats.
RESULTS: Mean age of the wild homozygous genotype CC, mutant homozygous genotype AA and heterozygous genotype CA was 1.38±0.49; 1.50±0.53 and 1.71±0.49 years respectively. Under the recessive model, the A1090E variant did not correlate with NSHSHL, evidenced by the odds ratio for mutant homozygous genotype AA at 0.23. The variant's genotype deviated from Hardy-Weinberg Equilibrium (p < 0.0001). Among 100 NSHSHL cases, 79, 13, and 8 exhibited wild genotype CC, mutant genotype AA, and heterozygous genotype CA, respectively. In the analysis of gender, A1090E variant in OTOF, females had no risk of deafness with heterozygous (OR=1.00) or mutant genotype (OR=0.27). Similarly, males exhibited no risk with CA and AA genotypes (OR=0.69 and 0.12).
CONCLUSION: Despite the detection of the otoferlin A1090E variant in both cases and controls, suggesting a protective role in hearing loss, it did not exhibit an association with disease risk in the study population.
KEYWORDS: A1090E variant (Non-MeSH); Hearing Loss (MeSH); Autosomal Recessive Hearing Loss (Non-MeSH); Non-syndromic Hearing Loss (Non-MeSH); Hearing Loss, Sensorineural (MeSH); Otoferlin (Non-MeSH); Cochlear Implants (MeSH); Pakistan (MeSH).
INTRODUCTION
Hearing is an important factor in being able to interact with others, exchange ideas and engage in different activities.1 Approximately 30 million people have ‘disabling’ hearing loss.2 By the year 2050 almost 2.5 billion people will have some degree of hearing loss, and at least 700 million will require hearing rehabilitation.2Around 80% of deaf people belong to low- middle-income countries.2 The prevalence of hearing loss in developed countries is much lower than its prevalence in developing countries.3 Deafness is most frequently caused by genetic factors, craniofacial abnormalities, and congenital infections.4 Prelingual hearing loss is a state that occurs when a child is either born deaf or loses his or her hearing ability in the early years of life before acquiring language. There is a need for early identification, assessment of hearing loss, and early rehabilitation in children.5 Autosomal dominant inheritance associated with hearing loss (HL) is considered post-lingual hearing loss, and progressive in nature. Whereas, autosomal recessive hearing lossis considered as pre-lingual hearing loss and nonprogressive in nature.6
In Pakistan, the consanguinity rate is approaching 70%, and hereditary hearing loss is a result of the high incidence of consanguineous marriages.7 Up till now, more than 120 genes have been related to non-syndromic hearing loss.8 Autosomal recessive non-syndromic hearing loss has been linked to more than 70 genes.9 Theotoferlin, (OTOF) encoding otoferlin is reported to be one of the major causes of NSHL.10 Mutations in otoferlin lead to profound hearing loss in humans.11 Otoferlin is a six C2 domain, a calcium binding transmembrane protein of the presynaptic vesicles present in the inner hair cells of the cochlea.12 Since its identification, approximately220 pathogenic and likely pathogenic variants ofotoferlin have been identified.8 One of the cohorts evaluated the genomic nucleotide sequence of OTOF and identified thepossible pathogenic variants among13 families Including fivemissense variants (p.L573R, p.A1090E, p.E1733K, p.R1856Q and p.R1939W).13Individuals with auditory neuropathy who suffered from severe to profound hearing lossor failed to respond with hearing-aids cochlear implant,14 serves as the only possible effective treatment. The site of the lesion in the case of the otoferlin mutation is supposed to be presynaptic. Hence, the function of the auditory nerve remains intact. Consequently otoferlin associated earing lossis expected to show a good cochlear implantoutcome.15
One of the pathogenic variants of otoferlin, A1090E, was found to be a risk factor in a Pakistani consanguineous family, responsible for autosomal recessive hereditary HL.13 Hypothesis of this study was that there is an association between the A1090E variant of the OTOF gene and the development of non-syndromic hereditary sensorineural hearing loss (NSHSHL) in people who received cochlear implants. There is no recent research available that may confirm the association of A1090E variant with non-syndromic hereditary hearing impairment in Pakistan. Therefore, this investigation will be helpful in the creation of a national genetic database for hereditary deafness and the provision of comprehensive genetic testing.
METHODS
This case-control population association based study was carried out from January 2022 to December 2022 in collaboration with the ENT Department of the Combined Military Hospital (CMH) Rawalpindi, Pakistan. This study comprised 100 cases of severe to profound NSHSHL who had undergone cochlear implant at ENT Department CMH Rawalpindi, and 100 healthy individuals recruited from CMH Rawalpindi. The disease group comprised of 100 individuals with severe to profound hearing loss, identified using standard audio logical procedures such as pure tone audiometry (PTA), tympanometry, brainstem evoked response audiometry, and auditory steady-state response (ASSR). For follow-up post cochlear implants, these cases were brought to the ENT outpatient clinic. A thorough history was collected in order to exclude out concomitant syndromic traits and acquired deafness factors.
We performed DNA extraction, polymerase chain reaction, and restriction fragment length polymorphism on blood samples taken from each participant in Center for Research in Experimental and Applied Medicine (CREAM) laboratory of the Department of Biochemistry and Molecular Biology, Army Medical College Rawalpindi. A formal approval from Ethical Review Committee of Army Medical College was obtained before commencement of the study (ERC/ ID/ 148, dated 17 January 2022).
In this case-control study, a non-probability purposive sampling technique was used with CI 95% 5% error of margin. Total sample size was 200, calculated by WHO sample size calculator with hearing loss prevalence of 0.12%.16Case group comprised 100 individuals up to age of 10 years, affected with NSHSHL with no other disorder, and who had received cochlear implant. Control group comprised 100 age- matched healthy individuals (both genders). After taking informed written consent, 02mlvenous blood samples were taken from all enrolled subjects.
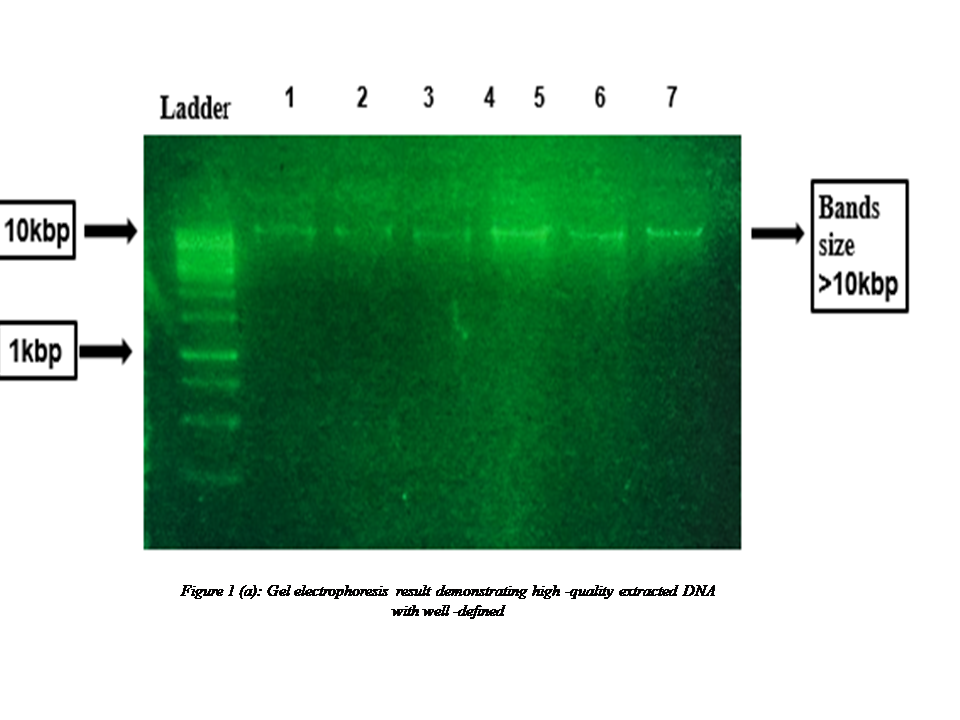
Molecular analysis: DNA was extracted using commercially Genomic DNA Extraction kit, (FAVORGEN BIOTECH ORPORATION, Cat. No.: FABGK 001). The DNA bands were resolved on 01% agarosegel are shown in Figure 1 (a).
 Information regarding the study gene OTOF, was
obtained from Online Mendelian Inheritance in Man (OMIM) available at (https://www.omim.org/entry/603681). Sequence of exon 27 of OTOF was
downloaded from Ensembl genome
browser available at (https://asia.ensembl.org/index.html). Primers for the
A1090E variant were designed using online bioinformatics tool Primer3Plus available
at (https://www.bioinformatics.nl/cgi-bin/primer3plus/primer3plus.cgi). The
sequence of A1090E forward primer was 5′-CTGAAGGGCCAGCAGGA-3′,
and reverse primer was 5′-
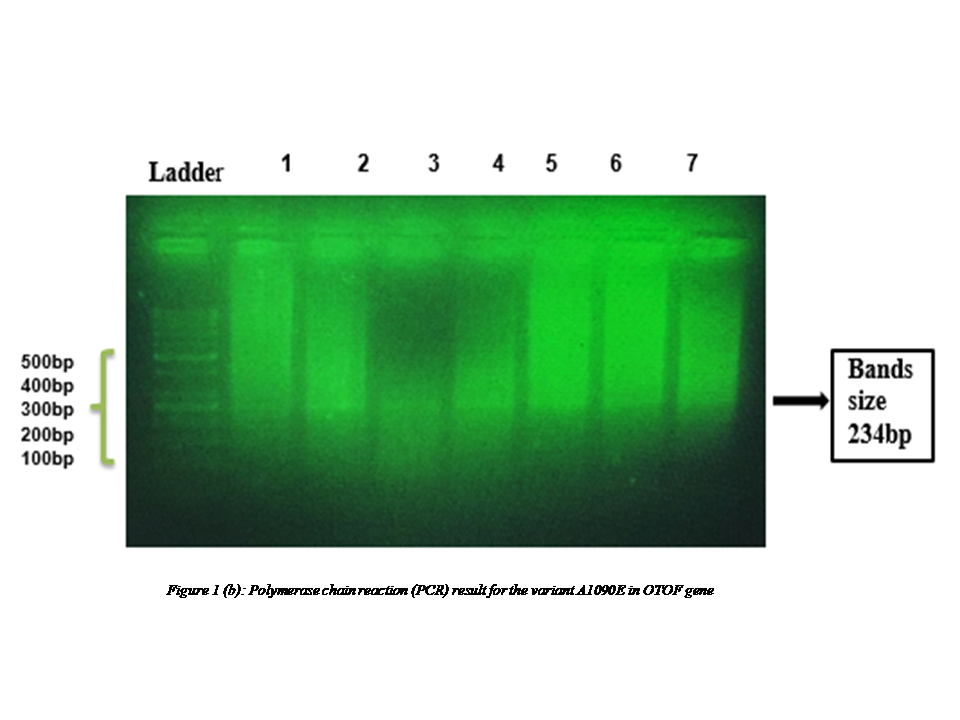
GAAGTCGTCAGCGGAGAAGT-3′with product size of 234bp.
Information regarding the study gene OTOF, was
obtained from Online Mendelian Inheritance in Man (OMIM) available at (https://www.omim.org/entry/603681). Sequence of exon 27 of OTOF was
downloaded from Ensembl genome
browser available at (https://asia.ensembl.org/index.html). Primers for the
A1090E variant were designed using online bioinformatics tool Primer3Plus available
at (https://www.bioinformatics.nl/cgi-bin/primer3plus/primer3plus.cgi). The
sequence of A1090E forward primer was 5′-CTGAAGGGCCAGCAGGA-3′,
and reverse primer was 5′-
GAAGTCGTCAGCGGAGAAGT-3′with product size of 234bp.
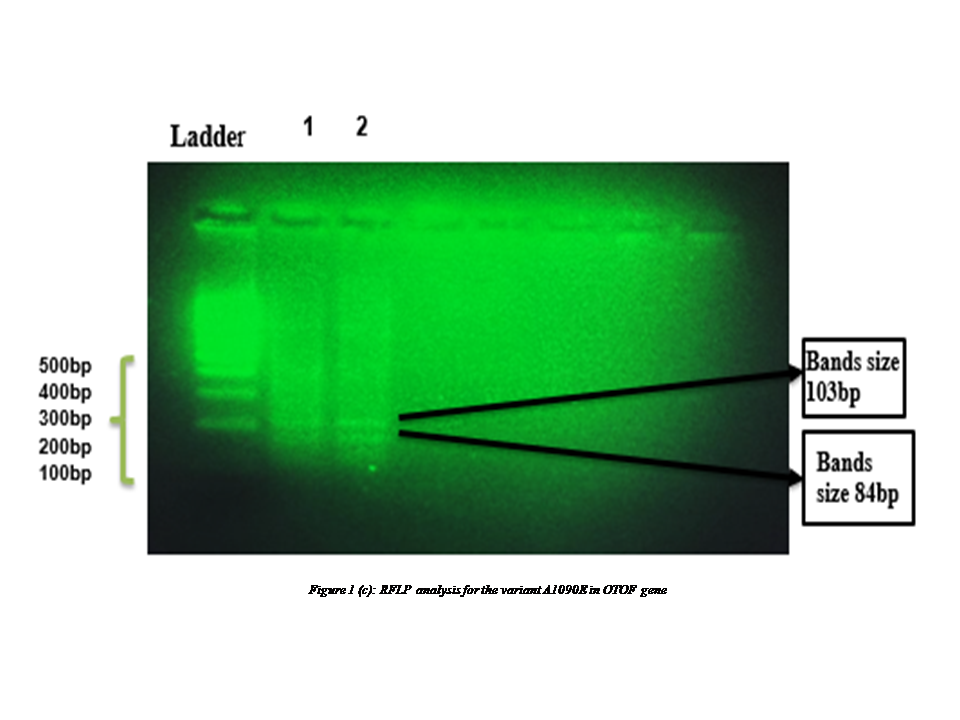
Polymerase chain reaction (PCR) was performed to amplify the gene of interest. The reaction mixture was prepared using(1X) Taq buffer 2.0μl, 0.2 mMol dNTPs mix, 1.5 mMolMgCl2, 01pmol/μl forward primer, 01pmol/μlreverse primer, 01 unit Taq DNA polymerase, 200ng DNA template, and 17μl nuclease free water. In total 25μl of reaction mixture was prepared. PCR parameters for variant A1090E were: hot start at 95℃ for 05 minutes, 35 cycles of denaturation at 95℃ for 30 seconds, annealing at 61.1℃ for 30 seconds, extension at 72℃ for 30 seconds, and final extension at 72℃ for 07minutes. The amplified PCR products were resolved on 02% agarose gel(Figure1 b). The amplified PCR products were digested using restriction enzyme Fast Digest Hin6I (Thermo Fisher Scientific, US Cat. No.: FD0484). The protocol comprised preparation of reaction mixture by using 10μl PCR product, 03μl of 10Xrestriction enzyme buffer, 16μl nuclease free water and 01μl Hin61 enzyme. The reaction mixture was incubated in water bath at 37ºC for 07 minutes and reaction was inactivated by incubation at 80ºC for 10 minutes. Lastly, gel electrophoresis with 02% agarose was performed to identify any genetic mutation (Figure1 c).
Statistical Analysis: Data was analyzed on SPSS (Version 22). Mean and± standard deviations were calculated for the qua
ntitative variables. Frequencies and percentages were calculated for analysis of the qualitative variables. The genotypes, allele frequency distribution and genetic models were analyzed using online bioinformatics SNP analysis tool i.e. SNP Stats available at: (https://www.snpstats.net/start.htm). Odds Ratio (OR= 95% CI) was computed by Pearson’s chi square test and logistic regression to conclude the association of the variant A1090E with the NSHSHL. To test for Hardy-Weinberg Equilibrium, exact test was applied, and p value < 0.05 was considered significant.
RESULTS
A1090E is a biallelic variant, having most common allele C and less common allele A. Allelic and genotypic frequencies in the two groups are given in Table-I. Allele frequency percentage, and genotype frequency percentage in study groups are shown in detail in Table I.
Table I: Allelic, genotypic frequencies and SNP exact test for Hardy-Weinberg equilibrium for the variant A1090E of otoferlin gene (N=200)
|
|
Genotypic Frequency |
Allelic Frequency |
SNP exact test |
|||
|
Groups |
CC |
CA |
AA |
C |
A |
|
|
Case |
79% |
8% |
13% |
83% |
17% |
p < 0.0001 |
|
Control |
89% |
4% |
7% |
91% |
9% |
p < 0.0001 |
SNP: Single Nucleotide Polymorphism
The p-value for Hardy-Weinberg Equilibrium was <0.0001 for A1090E variant in the both groups. In order to determine association of the A1090E with NSHSHL, different genetic models were adopted. These models along with Odds Ratios (95% CI) are shown in detail in Table II.
Table II: Genetic models used to study the association of A1090E with non-syndromic hearing loss (N=200, 95% CI, adjusted by age + sex).
|
Model |
Genotype |
Case |
Control |
OR (95% CI) |
P-value |
AIC |
BIC |
|
Codominant |
CC CA AA |
79 (79%) 8(8%) 13 (13%) |
89 (89%) 4 (4%) 7 (7%) |
1.00 0.73 (0.15-3.54) 0.22 (0.03-1.45) |
0.21 |
133.2 |
149.7 |
|
Dominant |
CC CA-AA |
79 (79%) 21 (21%) |
89 (89%) 11 (11%) |
1.00 0.42 (0.12-1.46) |
0.15 |
132.2 |
145.4 |
|
Recessive |
CC-CA AA |
87 (87%) 13 (13%) |
93 (93%) 7 (7%) |
1.00 0.23 (0.04-1.48) |
0.086 |
131.3 |
144.5 |
|
Over-dominant |
CC-AA CA |
92 (92%) 8 (8%) |
96 (96%) 4 (4%) |
1.00 0.84(0.18-4.01) |
0.83 |
134.2 |
147.4 |
|
Log-additive |
---------- |
---------- |
----------- |
0.52 (0.23-1.18) |
0.091 |
131.4 |
144.6 |
CI: Confidence Interval, OR:Odds Ratio, AIC: Akaike’s Information Criterion, BIC: Bayesian Information Criterion.
PCR and RFLP results for A1090E variant are shown in Figures1(b) (c) respectively.
 In
considering the sex and the A1090E variant of OTOF, females were not at risk
from either heterozygous genotype (OR=1.00) or mutant genotype (OR=0.27). In
males, the heterozygous genotypes CA and mutant genotype AA also did not impose
risk for deafness (OR=0.69 and 0.12 respectively).
In
considering the sex and the A1090E variant of OTOF, females were not at risk
from either heterozygous genotype (OR=1.00) or mutant genotype (OR=0.27). In
males, the heterozygous genotypes CA and mutant genotype AA also did not impose
risk for deafness (OR=0.69 and 0.12 respectively).
Mean age of the wildhomozygous genotype CC was found 1.38 ± 0.49 years. Mean age of the mutant homozygous genotype AA was found 1.50 ± 0.53 years. Whereas mean age of the heterozygous genotype CA was found 1.71 ± 0.49 years.
Wild homozygous genotype CC was found in 50% of male and 35% of female cases of NSHSHL. While only 06% of males and 02% of females were found to have the mutant homozygous genotype AA. Heterozygous genotype CA was found in 05% of male and 02% of female.
In wild genotype CC cases, the disease onset was prelingual in 80% of cases and postlingual in 05% of cases. In mutant genotype AA cases, the disease onset was prelingual in 07% of cases and postlingual in 01% of cases. While in heterozygous genotype CA cases, the disease onset was prelingual in all (07%)cases.
In wild genotype CC cases, the disease course was progressive in 11% of cases and non-progressive in 74% of cases. In mutant genotype AA cases, the disease course was progressive in 01% of cases and non progressive in 07% of cases. While in heterozygous genotype CA cases, the disease course was progressive in 01% of cases and non progressive in 06% of cases.
In considering the wild genotype CC, mutant genotype AA and heterozygous genotype CA cases parental first cousin marriages were found in 62%, 07%and 04% of cases respectively.
DISCUSSION
The results showed no association among the genotypes and alleles of A1090E of the otoferlin in the development of deafness in patients of NSHSHL. The allelic and genotypic frequency values and the genetic models adopted using the SNP Stats software revealed no significant association of the A1090E variant of OTOF with the development of NSHSHL.
Wild genotype CC was observed as a most common genotype in both groups and allele C was found as a most common allele in both groups. So the association of A1090E variant with the development of deafness in patients of NSHSHL cannot be assessed. Globally, various studies have been conducted that either deny or associate with the results of this study due to diverse ethnicities and different study population.13, 17
Allelic frequencies of the variant A1090E were in Hardy-Weinberg equilibrium of p + q=1. The p-value of <0.0001 indicated that the genotypic frequencies were not following Hardy-Weinberg Equilibrium which shows deviation due to chance.
For the association analysis of A1090E with NSHSHL, 04 genetic models were adopted; codominant, dominant, recessive and over dominant. Recessive model was considered as best genetic model on basis of smallest value of AIC and BIC calculated by genetic model. According to Log-additive homozygote CC was not associated with NSHSHL, while the heterozygote CA and mutant AA were protective.17
Parental consanguinity was 85-87.5% in mutant homozygous genotype AA and heterozygous genotype CA. One of the latest study conducted in Pakistan stated that consanguineous marriages in Pakistan are 73% and the country has the largest community of deaf children.18 Some studies have reported that non-syndromic hearing loss with autosomal recessive inheritance is observed in 75%-80%, and this type is particularly prevalent in consanguineous marriages.7 In this way the chances of being affected by the disease increases, when both parents carry the same recessive alleles.19
In considering the wild genotypes CC, mutant homozygous AA and heterozygous genotype CA, there was an overall increased male prevalence of hearing loss of 61%. According to one study that compared hearing loss in male and female participants, males had a far greater overall prevalence of hearing loss.20
In considering the wild genotypes CC, mutant homozygous AA and heterozygous genotype CA there was an overall increased incidence of prelingual onset of the disease, which was observed in 94% of cases. One of the studies stated that the presentation of hereditary hearing loss occurs in the early years of life.14 This highlights the need of early HL identification and treatment, as prompt intervention could help patients regain their speech and language abilities. All congenital HL has prelingual onset.9According to studies, the onset of autosomal recessive non-syndromic hearing loss is typically prelingual and nonprogressive until 5 years of age.21
This study has added new genetic data for hearing loss, helping to select variants for genetic testing, screening, and future research in hearing-related treatments. Sharing the results of this study with clinicians it could be helpful to establish pre-marital genetic screening of those at risk, similar to the current practice for thalassemia under Sindh Prevention and Control of Thalassemia Act, 2013. Furthermore, awareness campaigns about the detrimental consequences of cousin marriages among Pakistani families need to be initiated, as consanguinity is the main cause of hereditary hearing loss.
The study had limited sample size because of guardian reluctance for enrollment, financial constraints for genetic analysis and scarcity of cochlear implant centers in our country. So a study on a larger scale involving diverse ethnicities is recommended.
CONCLUSION
The otoferlin A1090E variant, present in both cases and controls, suggests a potential protective role against hearing loss in the study population. However, in cases with non-syndromic hearing loss, our findings indicate no association with disease risk. This dual presence of the variant underscores its complexity in contributing to auditory health, warranting further investigation into its nuanced impact on hearing outcomes.
REFERENCES
1. Wallhagen MI. The stigma of hearing loss. The Gerontologist2010;50(1):66-75.https://doi.org/10.1093/geront/gnp107
2. World Health Organization (WHO). Deafness and hearing loss; April 01, 2021. Accessed on:July 05, 2022. Available from URL: https://www.who.int/news-room/fact-sheets/detail/deafness-and-hearing-loss
3. Stevens G, Flaxman S, Brunskill E, Mascarenhas M, Mathers CD, Finucane M. Global and regional hearing impairment prevalence: an analysis of 42 studies in 29 countries. EurJ Public Health 2013;23(1):146-52.https://doi.org/10.1093/eurpub/ckr176
4. Iwasa YI, Nishio SY, Sugaya A, Kataoka Y, Kanda Y, Taniguchi M, et al. OTOF mutation analysis with massively parallel DNA sequencing in 2,265 Japanese sensorineural hearing loss patients. PLoS One 2019;14(5):e0215932.https://doi.org/10.1371/journal.pone.0215932
5. Jallu AS, Hussain T, Hamid WU, Pampori RA. Prelingual deafness: An overview of treatment outcome. Indian J Otolaryngol Head Neck Surg 2019;71(2):1078-89.https://doi.org/10.1007/s12070-017-1181-7
6. Van Laer L, McGuirt WT, Yang T, Smith RJ, Van Camp G. Autosomal dominant non-syndromic hearing impairment. Am JMedGenet 1999;89(3):167-74.https://doi.org/10.1002/(sici)1096-8628(19990924)89:3%3C167::aid-ajmg7%3E3.3.co;2-m
7. Ahmed S. Consanguineous Marriage and Its Impact on Hearing Impairment in Children. June 2022. Accessed on:July 05, 2022. Available from URL:https://www.researchgate.net/publication/361328115_Consanguineous_Marriage_and_Its_Impact_on_Hearing_Impairment_in_Children
8. Vona B, Rad A, Reisinger E. The many faces of DFNB9: relating OTOF variants to hearing impairment. Genes 2020;11(12):1411.https://doi.org/10.3390%2Fgenes11121411
9. Shearer AE, Hildebrand MS, Schaefer AM, Smith R. Genetic Hearing Loss Overview. 1999 Feb 14. In: Adam MP, Feldman J, Mirzaa GM, et al., editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993-2023. Accessed on:July 05, 202. Available from URL:https://www.ncbi.nlm.nih.gov/books/NBK1434/
10. Kuchay RA, Mir YR, Zeng X, Hassan A, Namba K, Tekin M. Novel OTOF pathogenic variant segregating with non-syndromic hearing loss in a consanguineous family from tribal Rajouri in Jammu and Kashmir. Int JPediatr Otorhinolaryngol 2020;130:109831.https://doi.org/10.1016/j.ijporl.2019.109831
11. Uthaiah RC, Hudspeth A. Molecular anatomy of the hair cell's ribbon synapse. J Neurosci 2010;30(37):12387-99.https://doi.org/10.1523/jneurosci.1014-10.2010
12. Michalski N, Goutman JD, Auclair SM, de Monvel JB, Tertrais M, Emptoz A, et al. Otoferlin acts as a Ca2+ sensor for vesicle fusion and vesicle pool replenishment at auditory hair cell ribbon synapses.Elife 2017;6:e31013.https://doi.org/10.7554/elife.31013
13. Choi BY, Ahmed ZM, Riazuddin S, Bhinder M, Shahzad M, Husnain T, et al. Identities and frequencies of mutations of the otoferlin gene (OTOF) causing DFNB9 deafness in Pakistan. ClinGenet 2009;75(3):237-43.https://doi.org/10.1111/j.1399-0004.2008.01128.x
14. Flint PW, Haughey BH, Robbins KT, Thomas JR, Niparko JK, Lund VJ, et al. CummingsOtolaryngology: Head and Neck Surgery e-book. Elsevier, United States; 2020.ISBN: 9780323612173
15. Zheng D, Liu X. Cochlear Implantation Outcomes in Patients With OTOF Mutations. Front Neurosci 2020;14:447.https://doi.org/10.3389/fnins.2020.00447
16. Pakistan Bureau of Statistics. Disabled population by nature of disability and sexcensus - 1998. Accessed on:July 05, 2022. Available from URL:https://www.pbs.gov.pk/sites/default/files/disability/disablity_data_1998.pdf
17. Naseer H, Rashid A, Majeed A, Baig ZA. Association of R1939W and P1987R variants of Otoferlin (OTOF) gene with severe to profound non-syndromic sensorineural hearing loss in Pakistani subjects. Pak J Med Sci 2023;39(5):1456-61.https://doi.org/10.12669/pjms.39.5.6393
18. Ralf A. Cousin marriage playing havoc with health in Pakistan. The News International.November 6, 2021. Accessed on:July 16, 2022. Available from URL:https://www.thenews.com.pk/print/906418-cousin-marriage-playing-havoc-with-health-in-pakistan
19. Gulani A, Weiler T. Genetics, Autosomal Recessive. [Updated 2023 May 1]. In: StatPearls[internet].Treasure Island (FL): StatPearls Publishing. Accessed on:July 16, 2022. Available from URL: https://www.ncbi.nlm.nih.gov/books/NBK546620/
20. Asghari A, Farhadi M, Daneshi A, Khabazkhoob M, Mohazzab-Torabi S, Jalessi M, et al. The Prevalence of Hearing Impairment by Age and Gender in a Population-based Study. IranJPublic Health 2017;46(9):1237-46.
21.Vona B, Doll J, Hofrichter MA, Haaf T. Non-syndromic hearing loss: clinical and diagnostic challenges. Medizinische Genetik 2020;32(2):117-29.https://doi.org/10.1515/medgen-2020-2022
|
Following authors have made substantial contributions to the manuscript as under:
IR: Concept and study design, acquisition, analysis and interpretation of data, drafting the manuscript, approval of the final version to be published AR& AM: Concept and study design, critical review, approval of the final version to be published KOKN & HGK: Acquisition, analysis and interpretation of data, critical review, approval of the final version to be published
Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work.
GRANT SUPPORT AND FINANCIAL DISCLOSURE Author declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |