![]() https://doi.org/10.35845/kmuj.2024.23415 ORIGINAL ARTICLE
https://doi.org/10.35845/kmuj.2024.23415 ORIGINAL ARTICLE
Comparison of Pilates exercises versus muscle energy technique with Kinesio taping in nonspecific low back pain: a randomized controlled trial
Anam Akram1,2, Kaynat Imtiaz 2, Shamoona Maryem 2,3,
Wajeeha Mahmood 2, Tahir Mahmood ![]() 2,4, Muhammad Naveed Babur2,5
2,4, Muhammad Naveed Babur2,5
|
1: CRC Department, Chaudhry Muhammad Akram Hospital, Superior University, Lahore, Pakistan 2: Department of Physical Therapy & Rehabilitation, Superior University, Lahore, Pakistan 3: Department of Physical Therapy & Rehabilitation, Services Hospital, Lahore, Pakistan 4: Department of Physical Therapy, University of Health Sciences, Lahore, Pakistan 5: Rashid Latif College of Physical Therapy, Rashid Latif Medical College, Lahore, Pakistan 6: Dean, Faculty of Allied Health Sciences, Superior University, Lahore, Pakistan
Email
Contact #: +92-300-6741320 Date Submitted: July 18, 2023 Date Revised: January 03, 2024 Date Accepted: January 06, 2024 |
|
THIS ARTICLE MAY BE CITED AS: Akram A, Imtiaz K, Maryem S, Mahmood W, Mahmood T, Babur MN. Comparison of Pilates exercises versus muscle energy technique with Kinesio taping in nonspecific low back pain: a randomized controlled trial. Khyber Med Univ J 2024;16(1):3-9. https://doi.org/10.35845/kmuj.2024.23415 |
ABSTRACT
OBJECTIVE: To compare the effects of Pilates exercise versus muscle energy technique (MET) along with Kinesio taping (KT) in nonspecific low back pain (LBP).
METHODS: This randomized controlled clinical trial was conducted from March 22 to September 14, 2022, at Chaudhry Muhammad Akram Research and Teaching Hospital, Johar Medicare Complex in Johar Town, Lahore, and Mayo Hospital and Jinnah Hospital in Lahore, Pakistan. Study involved 42 nonspecific LBP patients randomly assigned to group A (MET with KT) and group B (Pilates exercise with KT) over eight weeks after interventions. Pain, disability index, and range of motion (ROM) were assessed at baseline, 4 weeks and 8 weeks. Sessions were held twice a week, lasting 30-40 minutes each.
RESULTS: Among 42 participants, 14 (33.3%) were male, and 28 (66.7%) were female, aged 18-40 years. Group B showed greater pain reduction than group A (p<0.05). In group A, lumbar extension (p=0.10), lumbar rotation (0.18), right side flexion (0.02), and left side flexion (0.16) did not significantly improve. However, group B demonstrated improvements in flexion (0.04), extension (0.00), rotation (0.06), right side flexion (0.04), and left side flexion (0.08). The pain and disability improvement between groups exhibited a significant difference (p<0.05). ROM improvement also differed between groups (p<0.05), with group B showing dominant improvement.
CONCLUSION: Pilates exercise, combined with KT, demonstrated superior reduction in pain and improved range of motion compared to muscle energy technique with KT in nonspecific low back pain.
Clinical Trial Registration Number: NCT05352360
KEYWORDS: Exercise (MeSH); Kinesiotaping (Non-MeSH); Muscle Flexibility (Non-MeSH); Pilates (Non-MeSH); Muscle energy technique (Non-MeSH); Range of Motion, Articular (MeSH); Muscle Stretching Exercises (MeSH); Endurance (Non-MeSH); Functional movement (Non-MeSH); Quality of Life (MeSH); Low Back Pain (MeSH).
Low back pain (LBP), a prevalent and debilitating condition, spans from the 12th rib to the inferior gluteal folds.1 It manifests as either mechanical or non-mechanical in nature. The former can be nonspecific or specific.2 Approximately 85% of cases falling under the umbrella of non-specific LBP, often labeled as idiopathic low back dysfunction due to the absence of identifiable anatomical abnormalities. Heavy lifting combined with twisting or predictable spinal movements are common contributors to this condition.3 Highlighting its profound societal and economic repercussions, especially in developing nations, LBP stands as a significant driver of work absenteeism and disability, impacting between 60% to 80% of adults over their lifetimes.4 In Pakistan, the prevalence is notably high, ranging from 29.20% to 70% .5,6 Individuals experiencing low back dysfunction grapple with various musculoskeletal symptoms, including pain, restricted range of motion (ROM), diminished muscular strength activation, and a decline in functional indices.3
In the 1920s, Joseph Pilates introduced exercises designed to correct posture and strengthen lumbar pelvic muscles. These rehabilitative Pilates exercises, focusing on deep core muscles like multifidus, transversus abdominis, pelvic floor muscles, and the diaphragm,7 show promise in reducing pain and disability while improving motor functions of trunk muscles.8 Pilates exercises uniquely activate lumbar muscles and deep abdominals, promoting body conditioning by enhancing muscle strength, coordination, flexibility, and balance.9
Kinesiotaping (KT) is an effective rehabilitative technique, utilizing elastic tape stretched up to 140% of its original length. Applied over the injured skin or desired muscle, it enhances muscle strength, relieves pain, spasm, and edema, improving blood circulation and stabilizing joints for increased ROM.8,10 Different KT methods (I-shaped, Y-shaped, and Star-shaped) improve muscle tone, endurance, and proprioception, but further high-quality studies are needed to determine optimal efficacy.11 KT, when combined with squat exercises, has been studied for muscle strengthening in the lower extremities, demonstrating its effectiveness in reducing pain, decreasing disability, and improving ROM.12-14 Muscle energy technique (MET), a manual treatment involving contractions against counter forces, enhances muscle extensibility, joint ROM, and exhibits hypoalgesic effects on spinal pain.3,15
The primary research gap lies in the absence of prior comparisons between Pilates and MET in conjunction with KT for treating nonspecific LBP. This study employs a combined approach using Pilates, MET, and KT for nonspecific LBP, offering a more comprehensive strategy to address the multifaceted nature of the condition. This study was conducted to compare the effects of Pilates exercises versus MET along with KT in non-specific LBP aiming to reduce treatment time and disability within the community affected by LBP.
METHODS
This randomized controlled trial was conducted from March 2022 to 14 September 2022, after taking ethical approval from the Research Committee of Superior University Lahore (Ref # IRB/FAHS/DPT/1/23/A-13597). The study was registered as prospective with trial No. NCT05352360 and conducted according to CONSORT guidelines.
The sample size for this study was calculated by taking data from previous research. The visual analogue scale (VAS) is an outcome measurement tool along with µ1 and µ2. By using the following formula sample size was calculated:
n = [(z α/2+ zβ)2 x{2 (σ)²
}]
(µ1-µ2)
The sample size that was required in each group is mentioned as n. Z α/2 depends on the level of significance, for 5% this is 1.96. Zβ is dependent on power, for 80% this 0.8. 16 {Sakpal, 2010 #21}σ was the standard deviation which was 0.767. The mean change was µ1 in the VAS score for Pilates along with KT (group B) which was 4.00. The mean change was µ2 in the VAS score for the group A (MET along with KT) which is 4.66.4 Depending on the above information, the sample size required in each group was 21. The total sample size required to complete the study was 42, but with a 10% drop-out probability, we enrolled 46 patients. The sample was enrolled via the convenient sampling technique. Details of enrollment, intervention allocation, and follow-up of the patients is given in Figure 1.
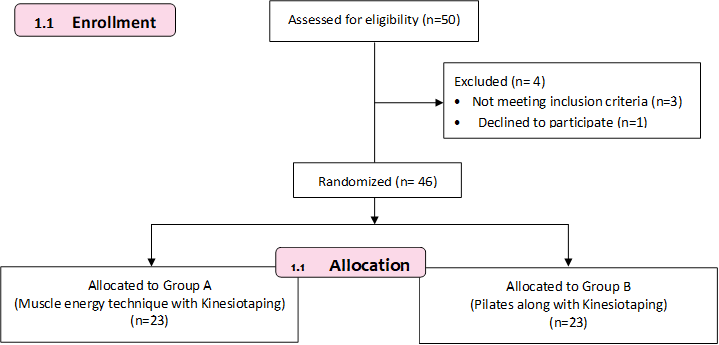
Figure 1: Flow chart showing enrollment, intervention allocation, and follow-up of patients
Data was collected at Chaudhry Muhammad Akram Research and Teaching Hospital (CMARTH) and Johar Medicare Complex in Johar Town, Lahore, as well as Mayo Hospital and Jinnah Hospital in Lahore, Pakistan.
All the ethics and research conducted for human subjects were followed, including the consent form, data confidentiality, and privacy of the subjects according to the Helsinki Declaration. The subjects were screened and subjects of both genders presented with non-specific LBP, between the age group of 18 and 40 years old, who can maintain their standing posture independently for ≥30 minutes, have enough physical autonomy to participate in the physical activities required by the study and have a pain intensity of 3 or greater.14 Subjects with any history of experiencing hypertension, ongoing pregnancy, spinal surgery, spondylol is thesis, sciatica, compression fracture, cardiovascular disease, liver disease, renal disease, diabetes mellitus, rheumatoid arthritis, or other rheumatologic-related pathologies7 taking corticosteroids 2 weeks before recruitment and hypersensitivity to the KT tape were excluded.3
Participants meeting the inclusion criteria were consecutively selected through a randomized lottery method. Subsequently, they were randomly assigned to both groups. The allocation process was concealed using the envelope method, ensuring the researcher remained unaware of the assignments. A blind assessor facilitated outcome assessments during both pre-treatment and post-treatment phases. The outcomes were pain intensity, ROM degrees, and disability. To measure pain, a VAS was used. Patients were instructed to rate their pain and describe their pain intensity by marking the point on the line that best shows symptom severity correspondence. 0–10 (0 = no pain and 10 = unbearable pain). The VAS correlations ranged from 0.60 to 0.77.17
The Oswestry Disability Questionnaire was used for measuring the level of disability in patients. This questionnaire consists of 10 categories, each of which scores on a scale of 0–5, where 0 shows no disability and 5 shows the greatest disability.11 Then scores were summed out of 50 scores. Each section carries five questions describing minimum to maximum levels of disability.18The Oswestry Disability Index (ODI) questionnaire is a reliable and valid tool with correlation values of r = 0.62 and ICC = 0.83. The test is considered the 'gold standard' of low-back functional outcome tools.14
Lumbar ROM was measured by using a universal goniometer with inter-observer reliability for goniometry in the thoracolumbar region (r = 1.0 Shober test to check reduction in range, r = 0.88 spinal extension, r = 0.76 right lateral spinal flexion, and r = 0.91 left lateral spinal flexion).19 In group A patients were given the MET, which includes manual treatment in which contractions are produced to control direction and position against the counterforce applied by the therapist to the patient.15
To implement the MET for the quadratus lumborum, an isometric contraction was initiated, followed by the patient relaxing after 7 seconds, and holding the end stretch for 30 seconds. For the erector spinae muscle, patients in a prone position raised their shoulders off the couch, maintaining this counter force for 7 seconds before relaxing. In the case of the iliopsoas muscle, patients lying on their back held their knee in position for 10 seconds before relaxing. To apply the technique on the tensor fascia latae, the patient in a supine position abducted the leg against applied resistance, sustaining this position for 10 seconds before relaxing.2
The objectives were to enhance ROM, alleviate muscle tension, and bolster muscle strength.20 For individuals with non-specific LBP, the MET protocol recommended an 8-week duration, twice a week, involving 3 repetitions with a 30-second hold.21 The KT method from Kenzokase's book was employed over the area of maximum lumbar pain, 11 applying Kinesio tape for 8 weeks, twice a week, with tape changes occurring every third day. Each tape, cut into a 5 cm width, utilized the star-shaped KT technique.
Two vertical strips were administered during trunk flexion, extending from the level of the posterior superior iliac spine to T12. While in an erect sitting position, horizontal Kinesio Tape strips were applied over both sides of the posterior superior iliac spine and on the erector spinae muscle with minimal tension in the tape. In the lower lumbar region, three I-shaped KT strips were applied, with the central part of the tapes overlapping without tension, and the outer portions applied with maximum tension (as illustrated in the Figure 2). The central portion of the tapes, where they overlap, was applied without tension, while the outer sections were affixed with maximum tension.14
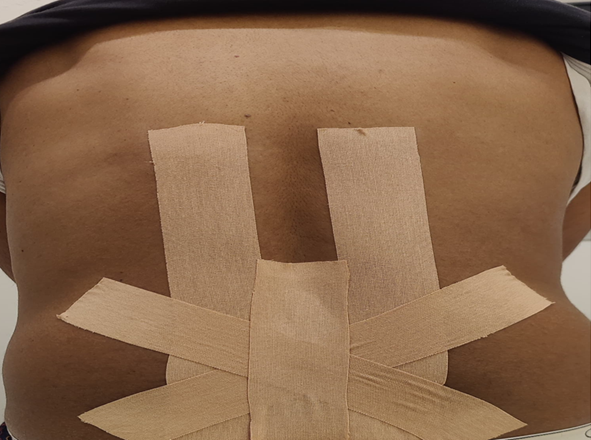
Figure 2: Kinesio Taping Method
In group B, participants engaged in Pilates exercises performed on a mat. These exercises included roll-up, bug leg, crook leg lying, prone single leg kick, side-lying clamshell, bug roll, knee/lumbar roll, and prone attitude rotation. For the roll-up exercise, participants began in a flat supine lying position, stretched their arms overhead, curved the upper and lower back to lift off from the mat, and touched their toes with their fingers. Bug leg exercise involved starting from supine lying with arms on the side, hip and knee flexed at 90 degrees, and concluding with terminal knee extension. Crook lying leg exercise started with the person lying flat, arms at the side, hip/knee bent with feet on a flat surface, and ended with terminal knee extension.
Prone single leg kick involved the participant being prone on a flat surface with hands supporting the forehead, bending one knee to 90 degrees, and raising the leg from the floor without compensatory trunk movement. Side-lying clamshell required lying on a flat surface on the non-tested leg with knees bent at 90 degrees and hips flexed at the assessed angle. The participant's hand palm supported the head, while the other hand was on the hip, abducting the above knee, and the assessor applied the break test of the manual muscle testing technique.
For bug roll exercise, the patient lay supine with arms abducted or stretched and flexed hip/knee at 90 degrees, rolling the knee about 30 to 45 degrees to one side, then returning to the back. In knee/lumbar roll, the person lying flat on their back with arms by the side, hips and knees bent, feet firmly on the floor, rolled their knees about 30 to 45 degrees to one side. Prone attitude rotation involved lying prone on a flat surface with hands supporting the forehead, bending one knee to 90 degrees, lifting the bent leg off the mat, and twisting to the contralateral side. The Pilates protocol spanned 8 weeks, with two sessions per week (totaling 16 sessions), each lasting 30 minutes, and comprising 10 repetitions.10
All patients received a standardized set of instructions following the intervention, with guidelines provided to minimize potential biases during reevaluation. This study upheld ethical considerations, ensuring no impact on patients' ethics, values, or cultural norms. The researcher adhered to ethical standards throughout each treatment session, with no violations observed during the entire study duration. Participants were granted the right to withdraw from the study at any time, emphasizing voluntary participation without any coercion.
Data analysis utilized SPSS 26, calculating mean ± SD for variables such as age and body mass index. Categorical variables, like gender, were represented in frequency. Normality was assessed through the Kolmogorov-Smirnov test and Shapiro-Wilk. Pain and disability results were presented as median and Interquartile Range (IQR) within groups using Wilcoxon signed ranks, and between-group comparisons employed the Mann–Whitney U test. ROM was expressed as mean ± SD based on normal distribution. Significance was set at p<0.05 (95% CI).
RESULTS
The mean age of participants was 29.95±7.09 years with age ranging from 18-40 years. Both groups were comparable at baseline in terms of age and gender with chronic non-specific LBP (p-value >0.05). Out of 42 participants, 14 (33.3%) were male and 28 (66.7%) were female participants. The mean weight was 67.28±15.68 Kg and the mean body mass index was 24.73±6.47 Kg/m2.
The within-group analysis showed that pain was more reduced in group B (Pilates+KT) compared to group A (MET+KT) with p –value <0.03 and 0.00 respectively. The disability index (ODI) showed median 10.5 with IQR of 7.75-15.0 (p value <0.05) with a statistically significant difference between both groups. The ROM in group A, where lumbar extension (p=0.10), lumbar rotation (p=0.18) and right side flexion (p=0.02) and left side flexion (p=0.16) were improved in group A but improved dominantly in group B for flexion (p=0.04), extension (p=0.00), rotation (p=0.06), right side flexion (p=0.04) and left side flexion (p=0.08) (Table I).
Table I: Within group comparison of pain, disability and range of motion
|
Outcomes |
Intervention |
Group A (N=21) |
P-Value |
Group B (N=21) |
P Value |
|
|
Pain |
At Baseline |
6.0 (5.0-7.0) |
0.03 |
6.0 (5.0-6.50) |
0.00 |
|
|
After 04 Weeks |
5.0 (3.5- 5.50) |
4.0 (3.0-5.0) |
||||
|
After 08 Weeks |
3.0 (2.00-3.50) |
1.0 (0.0-1.50) |
||||
|
Oswestry Disability Index |
At Baseline |
30.0 (22.5-35.0) |
0.00 |
28.0 (20.0-31.0) |
0.02 |
|
|
After 04 Weeks |
25.0 (19.5-30.0) |
20.0 (14.50-24.0) |
||||
|
After 08 Weeks |
15.0 (11.5-2.00) |
8.0 (5.0-10.0) |
||||
|
Thoraco Lumbar-Range of Motion (Degrees) |
Thoraco Lumbar Flexion |
At Baseline |
32.09±6.21 |
0.04 |
35.19±5.39 |
0.04 |
|
After 04 Weeks |
36.04±4.47 |
40.14±3.48 |
||||
|
After 08 Weeks |
41.42±2.90 |
45.09±1.64 |
||||
|
Thoraco Lumbar Extension |
At Baseline |
16.52±3.53 |
0.10 |
17.47±3.10 |
0.00 |
|
|
After 04 Weeks |
19.14±2.53 |
21.04±2.33 |
||||
|
After 08 Weeks |
21.76±1.70 |
24.19±.98 |
||||
|
Thoraco Lumbar Rotation |
At Baseline |
19.57±3.94 |
0.18 |
21.19±3.38 |
0.06 |
|
|
After 04 Weeks |
22.42±3.44 |
25.23±2.40 |
||||
|
After 08 Weeks |
25.33±2.37 |
28.90±1.30 |
||||
|
Thoraco Lumbar Right side flexion |
At Baseline |
16.47±2.46 |
0.02 |
16.95±1.71 |
0.04 |
|
|
After 04 Weeks |
19.42±2.27 |
20.23±1.51 |
||||
|
After 08 Weeks |
21.71±1.58 |
23.95±1.11 |
||||
|
Thoraco Lumbar left side flexion |
At Baseline |
16.71±2.59 |
0.16 |
16.80±1.93 |
0.08 |
|
|
After 04 Weeks |
19.52±2.58 |
20.42±2.06 |
||||
|
After 08 Weeks |
22.00±1.37 |
24.09±0.99 |
||||
Pain and Oswestry Disability Index are presented as Median and Inter Quartile Range, Thoraco Lumbar-Range of Motion is presented as Mean±SD; Wilcoxon Signed Ranks, range of motion is analyzed using repeated measurement ANOVA ,*p-value ≤ 0.05
The improvement in the pain and disability was statistically significant between both groups A and B (p<0.05). The improvement in the ROM was statistically significantly different between both the groups (p<0.05) with significant improvement in group B after 08 weeks of intervention (Table II).
Table II: Between Group Comparisons of Outcomes
|
Outcomes |
Groups (A and B) |
P-value |
|
|
Pain |
2.0(2.00-3.0) |
0.00 |
|
|
Oswestry Disability Index |
10.5 (7.75-15.00) |
0.00 |
|
|
Thoraco Lumbar-Range of Motion (Degrees) |
Flexion |
-3.66 |
0.00 |
|
Extension |
-2.42 |
0.00 |
|
|
Rotation |
-3.57 |
0.00 |
|
|
Right side flexion |
2.23 |
0.00 |
|
|
Left side flexion |
-2.09 |
0.00 |
|
Pain and Oswestry Disability Index are presented as Median and Inter Quartile Range, Thoraco Lumbar-Range of Motion is presented as Mean±SD; Mann–Whitney U test applied, ROM is analyzed using independent sample t test at *p-value < 0.05
DISCUSSION
This randomized controlled trial was conducted on a sample of 42 patients with nonspecific LBP to compare the effects of Pilates exercise and MET. The post-treatment group difference was significant over eight weeks of intervention for improving disability, pain, and ROM. Pilates along with Kinesio tape, was also more effective for improving pain, disability index, and ROM. The major outcome of this research was that eight weeks of Pilates and KT were effective in reducing pain and disability and enhancing ROM in patients with non-specific low back pain. As stated by Chong Kwok, that the clinical Pilates exercise gives us an alternative approach for the management of non specific LBP. This is an efficient and safe exercise that can be prescribed to the patient to improve their movement.9 The current research shows the same results in which Pilates had positive effects on improving the movement performance or disability of non-specific LBP patients. In another study on the effect of Pilate’s protocol on patients twice a week for eight weeks, there was a decrease in pain and reduction in disability scores in patients with nonspecific LBP, and improvements in resistance, flexibility, and muscular force.7
Despite current research showing limited benefits of MET in improving disability, ROM, and pain for nonspecific LBP, Thomas E, et al.,14 found it effective for asymptomatic and symptomatic patients. Further evidence is required to confirm its efficacy in muscular disorders. Dhargalkar found MET effective when combined with supervised exercises, resulting in faster recovery than exercise alone.2 Similarly, current research indicates MET's effectiveness, especially when combined with KT, in reducing pain and disability for nonspecific low back pain patients. In current research, KT demonstrated effective pain management without any therapeutic technique. However, it was included in both groups. Jung suggested adding KT for nonspecific LBP management.13 Guangchen found that combining KT with physical therapy yielded superior therapeutic effects, particularly in improving disability and reducing pain, compared to physical therapy alone in nonspecific LBP patients. 1
The results favored Pilates and MET for pain reduction, disability improvement, and enhanced ROM. However, Abbasi S, et al., suggested that Kinesio taping shapes (I, Y, star) enhance circulation, proprioception, and muscle tone.10 Current findings acknowledge their effectiveness, but the optimal method remains unclear, warranting further high-quality clinical studies for investigation. Our study indicated superior outcomes in pain, disability, and ROM management using KT alongside other physical therapy techniques for nonspecific LBP. However, Sheng Y, et al., reported that KT, whether used alone or combined with general therapies, demonstrated greater pain relief and improvement in non spescific LBP patients.21
In group B, Pilates effectively reduced pain and disability, improving ROM in nonspecific LBP patients. Ashtiani AA , et al., also demonstrated Pilates' effectiveness in reducing pain and improving ROM in individuals with LBP.22 The positive impact on muscle fiber recruitment and trunk muscle activation makes Pilates a clinically useful tool for LBP management.7 Additionally, Instrument-Assisted Soft Tissue Mobilization (IASTM) alongside stretching exercises has shown effectiveness in breaking adhesions causing low back pain.23,24 Cruz-Díaz D, et al., supported Pilates' positive effects on pain, disability, and kinesiophobia in nonspecific chronic LBP patients, with no observed adverse effects.25 The current findings align with results of El Gendy MH, et al.,26 favoring Pilates mat exercises over MET in LBP management.
The primary limitation is the lack of investigation into long-term effects. Additionally, the small sample size, uneven gender distribution, and limited technique dosage may impact findings. Future research should explore Pilates and Kinesio taping's prolonged effects, optimize technique dosage for quicker improvement in nonspecific LBP management, and consider alternative KT applications, such as I, Y, X, fan, web, or donut-shaped. Larger sample sizes are recommended for further studies.
The study revealed significant findings in favor of Pilates exercise along with KT, as evidenced by a greater reduction in pain and improved range of motion compared to the muscle energy technique along with KT. While both groups showed improvements in pain and disability indices, the Pilates exercise group demonstrated statistically significant superiority. This suggests that Pilates exercise, when combined with KT, may be a more effective intervention for nonspecific low back pain compared to muscle energy technique with KT. Further research and long-term follow-up studies are recommended to validate these findings and explore the sustained benefits of Pilates exercise in managing nonspecific low back pain.
Disclaimer:
The
head of the ethical committee is the author of the study.
REFERENCES
1. Sun G, Lou Q. The efficacy of kinesio taping as an adjunct to physical therapy for chronic low back pain for at least two weeks: A systematic review and meta-analysis of randomized controlled trials. Medicine 2021;100(49):e28170. https://doi.org/10.1097/MD.0000000000028170.
2. Dhargalkar P, Kulkarni A, Ghodey S. Added effect of muscle energy technique for improving functional ability in patients with chronic nonspecific low back pain. Int J Physiother Res 2017;5(3):2082-7. https://doi.org/10.16965/ijpr.2017.144
3. Elshinnawy AM, Elrazik RK, Elatief EE. The effect of muscle energy techniques versus cross (X) technique Kinesio taping to treat chronic low back dysfunction. Int J Ther Rehabil 2019;26 (2):1-8. https://doi.org/10.12968/ijtr.2017.0038
4. Manikandan P, Kumar GM, Rajalaxmi V, Priya C, Yuvarani G, Tharani G, Kamatchi K, Raj GM. Effectiveness of Pilates exercises on non-specific low back pain to determine pain and disability. Biomed 2021;41(4):825-9.
5. Arslan SA, Hadian MR, Olyaei G, Bagheri H, Yekaninejad MS, Ijaz S, et al. Prevalence and risk factors of low back pain among the office workers of King Edward Medical University Lahore, Pakistan. Phys Treat 2016;6(3):161-8. https://doi.org/10.18869/nrip.ptj.6.3.161
6. Yang CY, Tsai YA, Wu PK, Ho SY, Chou CY, Huang SF. Pilates-based core exercise improves health-related quality of life in people living with chronic low back pain: A pilot study. J Body Mov Ther 2021;27:294-9. https://doi.org/10.1016/j.jbmt.2021.03.006.
7. Alves MC, de Souza Neto RJ, Barbosa RI, Marcolino AM, Kuriki HU. Effects of a Pilates protocol in individuals with non-specific low back pain compared with healthy individuals: Clinical and electromyographic analysis. Clin Biomech 2020;72:172-8. https://doi.org/10.1016/j.clinbiomech.2019.12.009
8. González-Gálvez N, Marcos-Pardo PJ, Carrasco-Poyatos M. Functional improvements after a pilates program in adolescents with a history of back pain: A randomized controlled trial. Complement Ther Clin Pract 2019;35:1-7. https://doi.org/10.1016/j.ctcp.2019.01.006
9. Kwok BC, Lim JXL, Kong PW. The theoretical framework of the clinical pilates exercise method in managing non-specific chronic low back pain: A Narrative Review. Biology 2021;10(11):1096. https://doi.org/10.3390/biology10111096
10. Abbasi S, Hadian MR, Olyaei G, Ghotbi N, Bozorgmehr A, Rasouli O. Application of various methods of lumbar kinesio taping on pain and disability in patients with chronic low back pain: Narrative review. Arch Neurosci 2020;7(2). https://doi.org/10.5812/ans.99982
11. Kim H-H, Kim K-H. Effects of Kinesio Taping with squat exercise on the muscle activity, muscle strength, muscle tension, and dynamic stability of softball players in the lower extremities: A randomized controlled study. Int J Environ Res Public Health 2022;19:276. https://doi.org/10.3390%2Fijerph19010276
12. Grase M, Elhafez HM, Abdellatif MM, Genedi AF, Mahmoud MA. Effect of instrument assisted soft tissue mobilization versus kinesio tape for chronic mechanical low back pain: a randomized controlled trial. Physiother 2023;31(2):27-33. https://doi.org/10.5114/pq.2023.125742
13. Jung K-s, Jung J-h, In T-s, Cho H-y. Influences of Kinesio taping with therapeutic exercise in patients with low back pain. Healthcare 2021;9(8):927. https://doi.org/10.3390%2Fhealthcare9080927
14. Thomas E, Cavallaro AR, Mani D, Bianco A, Palma A. The efficacy of muscle energy techniques in symptomatic and asymptomatic subjects: a systematic review. Chiropr Man Therap 2019;27:35. https://doi.org/10.1186/s12998-019-0258-7
15. Sakpal TV. Sample size estimation in clinical trial. Perspect Clin Res 2010;1(2):67-9.
16. Boonstra AM, Schiphorst Preuper HR, Reneman MF, Posthumus JB, Stewart RE. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int J Rehabil Res 2008;31(2):165-9. https://doi.org/10.1097/MRR.0b013e3282fc0f93
17. Grönblad M, Hupli M, Wennerstrand P, Järvinen E, Lukinmaa A, Kouri JP, et.al. Intercorrelation and test-retest reliability of the Pain Disability Index (PDI) and the Oswestry Disability Questionnaire (ODQ) and their correlation with pain intensity in low back pain patients. Clin J Pain 1993;9(3):189-95. https://doi.org/10.1097/00002508-199309000-00006
18. Fitzgerald GK, Wynveen KJ, Rheault W, Rothschild B. Objective assessment with establishment of normal values for lumbar spinal range of motion. Phys Ther 1983;63(11):1776-81. https://doi.org/10.1093/ptj/63.11.1776
19. Suresh AM, Kashyap D, Behera TP, Tarsolia KA. Effect of muscle energy technique in patients with non-traumatic lumbo-pelvic pain in the age group of 30-40 years. J Phy Med Rehab Stud Rep 2021;3(2):1-9 https://doi.org/SRC/JPMRS/138.2021:3
20. Patel VD, Eapen C, Ceepee Z, Kamath R. Effect of muscle energy technique with and without strain-counterstrain technique in acute low back pain - A randomized clinical trial. Hong Kong Physiother J 2018;38(1):41-51. https://doi.org/10.1142/S1013702518500051
21. Sheng Y, Duan Z, Qu Q, Chen W, Yu B. Kinesio taping in treatment of chronic non-specific low back pain: a systematic review and meta-analysis. J Rehabil Med 2019;51(10):734-40. https://doi.org/10.2340/16501977-2605
22. Ashtiani AA, Askari A. Effects of modified pilates exercises on pain, disability, and lumbopelvic motor control in patients with chronic low back pain. Phys Ther J 2020;10(4):195-204. http://dx.doi.org/10.32598/ptj.10.4.72.5
23. Mahmood T, Hafeez M, Ghauri MW, Salam A. Instrument assisted soft tissue mobilization-an emerging trend for soft tissue dysfunction. J Pak Med Assoc 2021;71(3):977-81. https://doi.org/10.47391/JPMA.1168
24. Mahmood T, Afzal W, Ahmad U, Arif MA, Ahmad A. Instrument soft tissue mobilization integrated with exercise for musculoskeletal disorders. Rawal Med J 2021;46(3):749-52.
25. Cruz-Díaz D, Romeu M, Velasco-González C, Martínez-Amat A, Hita-Contreras F. The effectiveness of 12 weeks of Pilate’s intervention on disability, pain and kinesiophobia in patients with chronic low back pain: a randomized controlled trial. Clin Rehab 2018;32(9):1249-57. https://doi.org/10.1177/0269215518768393
26. El Gendy MH, Hekal HN, Kadah MA, Hussein HM, Ewais NF. Pilate mat exercise versus muscle energy technique on chronic non specific low back pain. Int J Health Sci 2022;6(S5):3570-83. https://doi.org/10.53730/ijhs.v6nS5.9429
Following author have made substantial contributions to the manuscript as under: AA & KI: Study design, acquisition of data, drafting the manuscript, approval of the final version to be published SM: Analysis and interpretation of data, critical review, approval of the final version to be published WM: Concept and study design, critical review, approval of the final version to be published TM: Analysis and interpretation of data, drafting the manuscript, critical review, approval of the final version to be published MNB: Acquisition of data, drafting the manuscript, approval of the final version to be published Author agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work.
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |