![]() https://doi.org/10.35845/kmuj.2024.23373 CASE
REPORT
https://doi.org/10.35845/kmuj.2024.23373 CASE
REPORT
The inhibition of sertraline-induced serotonin syndrome by inadvertent co-ingestion of risperidone in a suicidal attempt: a case report
Marwan Saad Azzubaidi ![]() 1, Rosliza Yahaya
1, Rosliza Yahaya![]() 2, Harmy Mohamed Yusoff
2, Harmy Mohamed Yusoff ![]() 3
3
|
1. Department of Pharmacology, Faculty of Medicine, Universiti Sultan Zainal Abidin (UniSZA), Malaysia 2. Department of Pharmacology, Faculty of Medicine, UniSZA, Malaysia 3. Department of Pharmacology, Faculty of Medicine, UniSZA, Malaysia
Email
Contact #: +60-189-066351 Date Submitted: May 23, 2023 |
|
THIS ARTICLE MAY BE CITED AS: Azzubaidi MS, Yahaya R, Yousoff HM. The inhibition of sertraline-induced serotonin syndrome by inadvertent co-ingestion of risperidone in a suicidal attempt: a psychiatric case report. Khyber Med Univ J 2024;16(3):263-5. https://doi.org/10.35845/kmuj.2024.23373 |
ABSTRACT
BACKGROUND: Suicidal thoughts and attempts are commonly observed among patients with depression. The presence of concomitant psychotic symptoms in a patient with an existing depression increases the risk of drug-drug interactions, especially in cases when multiple drugs are used for treatment.
CASE PRESENTATION: This case report describes a young adult female with a history of psychosis and depression, for which she had been taking risperidone and sertraline for the past six months. She was brought to the hospital by her family members after an alleged suicide attempt using her psychiatric medications. On examination, the patient exhibited disturbed consciousness and a moderately elevated body temperature, but notably, no muscle rigidity.
These clinical features suggested a mild form of serotonin syndrome (SS). Despite a 1500 mg sertraline overdose, which would typically result in symptoms such as severe agitation, hallucinations, sweating, flushing, or tremors, the patient's SS was unexpectedly mild considering the amount of drugs ingested.
CONCLUSION: It was concluded that the patient developed serotonin syndrome (SS) due to a toxic overdose of sertraline. However, the severity of SS was mitigated by the concurrent ingestion of an equivalent dose of risperidone, a serotonin receptor antagonist. As a result, the condition was classified as mild to moderate SS, which, despite the large dose of the selective serotonin reuptake inhibitor, did not necessitate the use of an antidote.
KEYWORDS: Antidotes (MeSH); Sertraline (MeSH); Serotonin Syndrome (MeSH); Risperidone (MeSH); Suicide (MeSH); Suicide, Attempted (MeSH); Psychiatry (MeSH); Mental Disorders (MeSH).
INTRODUCTION
CASE PRESENTATION
The patient recently reported extreme stress and irritability following conflicts with her new boyfriend, which had caused her sleeplessness. In frustration, after three days of alleged continuous insomnia, she ingested two strips (20 tablets) of her prescribed medications in an attempt to sleep. The ingested drugs included equal amounts: ten tablets of sertraline (1500 mg) and ten tablets of risperidone (10 mg), taken simultaneously. She denied experiencing any depressive symptoms, hallucinations, delusions, or suicidal ideation at the time of the incident, which occurred while she was alone in her bedroom.
A few minutes after ingesting the tablets, the patient started experiencing dizziness and confusion. She was later found unconscious in the bathroom by her family members after failing to respond to their repeated phone calls. Upon admission to the hospital emergency department, she had three episodes of vomiting containing undigested pills and fluids. On further questioning, she reported palpitations, excessive sweating, and headaches, with no history of drug abuse. However, she did not experience diarrhea, shortness of breath, tremors, or jerky movements.
On examination, her blood pressure was 90/55 mmHg, and her Glasgow Coma Scale score was 13/15. Multiple cut wound scars were noted on her left wrist. A chest X-ray and an urgent brain CT scan were performed to rule out chest infections and intracranial bleeding, respectively. Supportive management was initiated, including oxygen administration via nasal cannula and intravenous noradrenaline to elevate her blood pressure. Eight hours later, she was admitted to the medical ward and placed in an acute care cubicle for close observation. Hourly blood pressure monitoring was conducted, and intravenous normal saline was administered to raise her blood pressure and compensate for fluid and electrolyte losses due to repeated episodes of spontaneous vomiting, which had a clear consistency.
During the first 24 hours of hospitalization, the patient developed a fever (38.2 °C) associated with rigor. However, she did not exhibit signs of agitation, neck stiffness, photophobia, or muscle aches. The fever resolved by the third day of admission. Throughout this period, her blood pressure was closely monitored and remained within the lower normal range. On the third day of hospitalization, the patient developed leukocytosis (16.6 × 109/L) without accompanying neck stiffness or other clinical signs of infection. Her plasma acetaminophen level was measured and found to be below the toxicity threshold, according to the Rumack-Matthew Nomogram.
The patient demonstrated poor insight into her psychiatric illness. While she was aware of her symptoms, she did not recognize that these were related to a mental health disorder, nor did she understand the necessity of treatment. The psychiatric team noted a history of poor medication compliance and frequent missed follow-up appointments since the initiation of her treatment.
DISCUSSION
Figure 1 illustration showing the difference in the effects of a sertraline SSRI overdose: (A) In the absence of a 5-HT2A receptor antagonist, leading to serotonin syndrome, characterized by exaggerated activity of postsynaptic serotonin receptors. (B) In the presence of a 5-HT2A receptor antagonist (such as risperidone), which inhibits excessive serotonin binding to postsynaptic 5-HT receptors.
In this case report, the patient was receiving sertraline, an antidepressant, along with a daily dose of risperidone for the management of concomitant psychosis. While risperidone is primarily used as an antipsychotic, it is known to carry a risk of inducing neuroleptic malignant syndrome (NMS),¹ a condition that shares clinical features with serotonin syndrome (SS), making differentiation between the two complications challenging.³ Consequently, the differential diagnosis in such a presentation includes NMS, particularly given the history of concurrent overdose involving both medications.
The factors supporting a diagnosis of SS rather than NMS, include the acute onset of symptoms such as fever with rigors, dizziness, palpitations, vomiting, and hypotension, alongside muscle rigidity, all occurring immediately after the overdose. The absence of hyporeflexia, a hallmark feature of NMS, further argues against an NMS diagnosis. Although both SS and NMS may present with elevated white blood cell (WBC) counts, this is considered a nonspecific finding.⁴
Considering the high dose of sertraline (1500mg) consumed by the patient, a more severe presentation of SS, including hyperthermia, respiratory depression, convulsion, and muscle rigidity, was anticipated.5 Surprisingly, in this case, the clinical features of SS ranged between mild to moderate severity. This relatively mild presentation of SS could be attributed to the pharmacological effects of the second drug taken in overdose-risperidone. Being a second-generation antipsychotic, risperidone primarily acts by inhibiting serotonin 5-HT2A receptors more so than blocking dopamine D2 receptors. This mechanism may have inadvertently limited the excessive binding of serotonin to postsynaptic receptors (Figure 1B).
Hence, we propose that risperidone may ‑have served as an incidental yet beneficial antidote, mitigating the severity of serotonin toxicity and eliminating the need for additional serotonin receptor antagonists. Additionally, the patient's repeated vomiting episodes likely reduced the gastrointestinal absorption of the drugs, further decreasing their systemic impact.
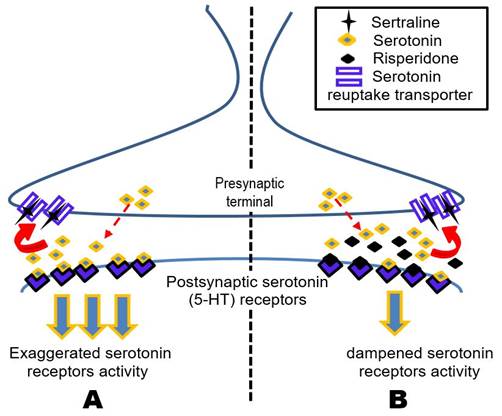
Figure 1. An illustration depicting the difference in the effect of excessive (overdose) sertraline SSRI, (A) in the absence of 5-HT2A receptor antagonist leading to serotonin syndrome, manifested by exaggerated postsynaptic serotonin receptors activity. (B) in the presence of a 5-HT2A receptor antagonist risperidone), which inhibits the excessive serotonin binding to postsynaptic 5-HT receptors, thereby preventing the progression in the severity of serotonin syndrome.
REFERENCES
2. Duignan KM, Quinn AM, Matson AM. Serotonin syndrome from sertraline monotherapy. Am J Emerg Med 2020;38(8):1695.e5-e6. https://doi.org/10.1016/j.ajem.2019.158487
3. Volpi-Abadie J, Kaye AM, Kaye AD. Serotonin syndrome. Ochsner J 2013;13(4):533-40.
4. Chandrasekaran P, Grewal G. An approach to diagnosing and managing neuroleptic malignant syndrome, atypical neuroleptic malignant syndrome, and serotonin syndrome using a flowchart algorithm. Austin J Pharmacol Ther 2015;3(2):1072. https://doi.org/10.1080/10673220701551110
5. Buckley NA, Dawson AH, Isbister GK. Serotonin syndrome. BMJ 2014;348. https://doi.org/10.1136/bmj.g1626
Following authors have made substantial contributions to the manuscript as under:
MSA: Diagnosis of the case, drafting the manuscript, critical review, approval of the final version to be published. RY: Identification and management of the case, drafting the manuscript, critical review, approval of the final version to be published. HMY: Management of the case, critical review, approval of the final version to be published. Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work.
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |