![]() https://doi.org/10.35845/kmuj.2023.23348 SYSTEMATI REVIEW
https://doi.org/10.35845/kmuj.2023.23348 SYSTEMATI REVIEW
Virtual reality intervention in lower limb locomotor training for patients with multiple sclerosis: a systematic review
Kholood Matouq
Shalabi1![]()
|
1: Department of Rehabilitation Sciences, College of Health and Rehabilitation Sciences, Princess Nourah bint Abdulrahman University, Riyadh, Kingdom of Saudi Arabia
Email
Contact #: +966-599-529625 Date Submitted: May 11, 2023 Date Revised: August 28, 2023 Date Accepted: August 31, 2023 |
|
THIS ARTICLE MAY BE CITED AS: Shalabi KM.Virtual reality intervention in lower limb locomotor training for patients with multiple sclerosis: a systematic review. Khyber Med Univ J 2023;15(4):258-69. https://doi.org/10.35845/kmuj.2023.23348 |
ABSTRACT
OBJECTIVE: To assess the results of virtual reality rehabilitation (VRR) use in locomotor training of lower limb motor skills for people with multiple sclerosis (MS).
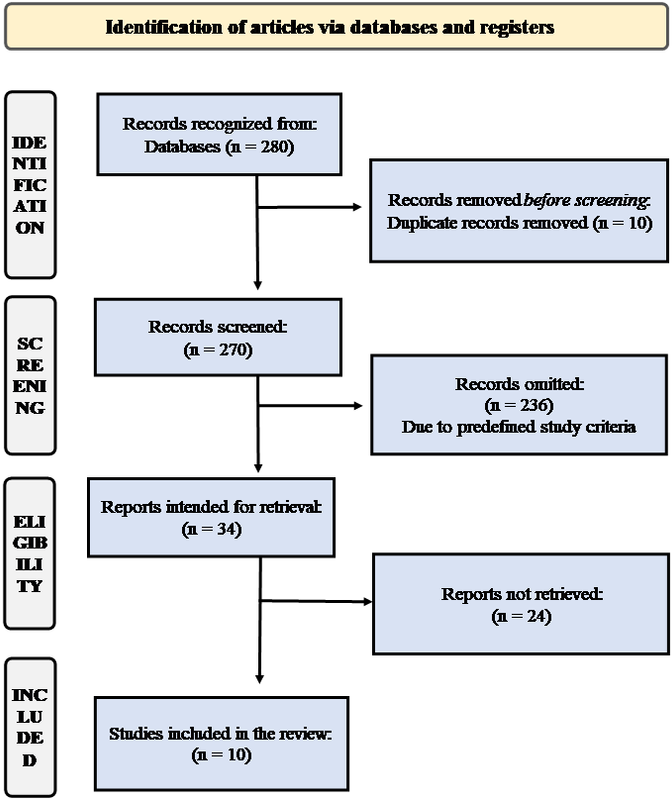
METHODS: This systematic review was done in accordance with the PRISMA guidelines. The literature search was done using Embase, MEDLINE, Physiotherapy Evidence Database (PEDro) and Google Scholar and articles from 1947 to 8th May 2020 were included. The keywords were “virtual reality”, “motor learning” and “Multiple Sclerosis”. The identified studies were screened in accordance with the inclusion criteria and pertinent data was retrieved. Studies included diagnosis of MS on McDonald criteria and with use of VR for rehabilitation were included.
RESULTS: The results included a total of 10 studies in the systematic review. These included five Randomized Controlled Clinical Trials, two prospective interventional studies, one cross-sectional study, one retrospective study, and one case series. The combined number of subjects from all studies included 376 patients diagnosed with MS. The research studies were published from 2007-2020. The review identified that VR paired with robot-assisted walk training significantly increased participants' 2-minute walk test scores and Paced Auditory Serial Addition Task scores compared to controls for the 10-meter walking test.
CONCLUSION: Virtual reality may have positive benefits on MS patients' quality of life and lower limb learning and function along with improvements in the cognitive abilities.
KEYWORDS: Virtual Reality (MeSH); Lower Limb (MeSH); Lower
Extremity (MeSH);Multiple Sclerosis (MeSH); Motor learning (Non-MeSH);
Neuromuscular illness(Non-MeSH); Video Games (MeSH).
INTRODUCTION
Multiple sclerosis (MS) is a complex illness of the central nervous system (CNS), with an estimated 2.8 million people living with MS.The incidence rate worldwide is 2.1 per 100,000 populations per year.1 The burden has significant impact of the cost of rehabilitation of these patients. In the developing countries the prevalence this is huge burden on the individuals where the there is no social security system in the country.
Presentation of MS varies from a minor condition to severe disability. Even those with minor disability, MS run the risk of having restricted ambulation.2Furthermore, asymmetries in gaitincluding increase in the limb support time, reduced speed and stride length are the major issues faced by MS patients. In addition, pervasive cognitive deficits are common in the form of deranged information processing speed, concentration, and cognitive capabilities are symptoms of mobility MS.3,4 Deterioration in the physical abilities along with the unpredictable and variable progressive nature of the disease, make it necessary to use human or technological assistance to perform routine daily tasks. In hospitals and specialized facilities, numerous MS neurological disease complications are treated as outpatients. However, the majority of MS patients experience mobility, geographic, or both limitations that prevent them from receiving therapy at a rehabilitation facility. As a result, there is rising interest in developing fitness efforts for MS patient rehabilitation.5,6
In the recent advancements virtual reality (VR) is an effective tool for improving real-world mobility in individuals with flexibility deficit, as it can imitate real-world obstacles and provide adjusted performance feedback.7Users can connect with computers by using their senses to explore virtual worlds with the help of several sensory channels. The term "immersion" describes how fully a person feels involved or immersed in a virtual world. Regarding human behavior and cognition, VR offers a variety of applications in technology, industry, education, and health, where it is crucial for both medical assessment and treatment as well as for intellectual assessment and therapy. VR can be used to develop training and testing environments for people that allow for the precise manipulation of complex incentive performances, allowing for accurate representations and the rehabilitation of human cognitive and functional performance.8
By its capacity to provide adjusted performance feedback and imitate real-world obstacles, VR is an effective technique for improving real-world mobility in patients with flexibility deficit.7 Users can explore virtual environments via a variety of sensory pathways, making it possible to get help form the VR mode of treatment. Gains in functional and brain reconfiguration can only be achieved with the use of cutting-edge rehabilitation techniques that require extensive task-specific practice, such as constraint-induced movement therapy (CIMT), robotics, and virtual reality training.9 Shalabi conducted a review of the empirical literature and concluded that that healthy people with a non-dominant hand tended to learn motor skills more effectively than those with a dominant hand in terms of practice, transfer, and learning.10,11
The results of many studies on MS patients who underwent diverse levels of trainings have shown improvements in head control14, gait13, and upper limb function, from minutes to few days.12 These studies also found the ability to create new motor skills were intact in the early stages of MS15, that may be compromised in more advance stages of MS.8 To enhance the learning of sequential events, such as spatial and temporal control, for rehabilitation among stroke patients, a custom video game technology was presented.16 In neuro-rehabilitation, VR has also been used as an active treatment tool.17Video games and automated analysis tools, according to Davison et al., can speed up the evaluation of rehabilitation strategies.18
VR can help with high-intensity, task-oriented multisensory feedback training when it comes to motor learning. The utility of a VR approach for balance and gait training in stroke patients19–21, Parkinson disease patients22 and older individuals22–25 has been thoroughly evaluated in severalrigorous studies and meta-analyses. However, the role of VRin locomotor training to improve motor learning in MS patients is limited. Furthermore, to the knowledge of the author there are no systematic review available of the topic. Therefore, the aim of this systematic review to assess the studies on motor learning with VR environment in MS patients. The purpose of the systematic review was to assess the evidence supporting the use of VR technology to assist patients with postural control problems during neurological rehabilitation.
METHODS
Literature search
The literature was systematically searched according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) criteria for conducting this systematic review.26For the determination of virtual reality and locomotor function in MS a review was conducted for numerous databases such as Embase, MEDLINE, Physiotherapy Evidence Database (PEDro) and Google Scholar from 1947 to 8th May 2020. Figure 1 presents the PRISMA flow literature search and the comprehensive research process (Figure 1).For the identification of studies, various terms like “virtual reality”, “virtual reality exposure therapy/virtual reality therapy/computer interface”, “video game/ gaming”, “balance/postural balance/postural control”, “walking/motor skills/motor learning/motor activity and “multiple sclerosis” were combined. The inclusion criteria for the systematic review were all the data considering virtual reality therapy used in motor skills improvement in multiple sclerosis patients. Only studies written in the English language were included. All the randomized control trials and prospective studies were included. The exclusion criteria were animal-based studies, duplicate publication, general review studies, and book chapters. There were four phases for the screening and selection of studies. These include identification, screening, eligibility, and inclusion. Two independent researchers examined the titles and abstracts. The papers that were determined to be pertinent based on the standards; the same two reviewers screened the full-text. Senior writers were contacted to resolve any differences in order to qualify the inclusion. Studies with individuals who had received a medical diagnosis of MS based on the updated McDonald criteria were included. In addition, an Extended Infirmity Status Scale of 6 (Ability to move 100 meters at a minimum when resting or using one twig or support) were included. Studies with individuals having other neurological or musculoskeletal issues, uncorrected eyesight problems that interfered with walking, or those who were severely injured were excluded. Furthermore, articles with any training for motor learning using any VR system and skill acquisition, inter-limb learning transfer, learning retention in lower limbs and learning transfer (or learning generalization) were thoroughly evaluated.
Data extraction
The same two reviewers extracted the data out. The study characteristics, publication year, study position, sample size, participant age, gender, level of disability, period of illness, study design, learning task type, intervention, comparator, outcome variables, and results of the outcome measures were all included in the data extraction sheets. Any disagreements on the withdrawal of a document were settled through consensus or by involving a senior researcher.
RESULTS
In this review study, a total of 280 articles were searched in different databases search. There were 10 duplicates found from different databases after searching the titles. Further, abstracts were screened and additionally 236 were rejected based on the inclusion and exclusion criterion. Thirty-four studies were subsequently subjected to full-text screening, 24 of which were disregarded due to unavailability of the full text retrieval. Eventually, this systematic review comprised of 10 studies. Because of the diverse study methods of the manuscript, and lackof comparison analysis, only the descriptive analyses of the retrieved articles were reviewed. Detail features and methods of the studies selected are given in Table I. This review comprised of 10 studies with 376 participants and include drandomized control trials (n=5), prospective interventional studies (n=2), cross-sectional studies (n=1), retrospective study (n=1), and case series (n = 1) were the types of studies. Due to the high levels of heterogeneity in all PICOS (Population, Intervention, Comparison, Outcomes, and Study) characteristics of the trials were compared.
Characteristics of the included studies and participants
Most of the studies (n = 6; 60%) were from Italy, with the remaining studies (n = 1) from Jordan, Spain, Turkey, and the United States. The studies were released between 2007 and 2020.The characteristics of the included studies are listed in Table I.
Features of interventions or VR systems
The intervention group made use of non-immersive, semi-immersive, and immersive systems, as well as computer-assisted rehabilitation systems, robot-assisted gait training, treadmill training, motor-tracking tasks, home-based intervention, and tele-rehabilitation treatment.11, 27-34Depending on the nature and viability of the study, the control group had regular physical treatment, conventional rehabilitation, exercise, regular treadmill training, or no intervention. With the aid of disease and region-specific scales, the effectiveness of VR for the patients was evaluated. Table II gives a thorough overview of VR.
Motor skill performance
The results in the improvement of motor skills performance is variable among different articles. In terms of VR gaming, Al-Sharman et al. found no significant differences (p = 0.8) between the groups. For the purpose of enhancing motor abilities, however, tele-rehabilitation management using an Xbox 360 console under videoconference supervision was remarkably successful.32As comparison to the control, the motor-tracking task utilizing a VR object produced improved performance in all planes, depth planes, and frontal planes.12The control trunk test and timed up-and-go test, which measure locomotor function, showed that semi-immersive VR did not improve it, although the Tinetti score was higher (P = 0.00) in the intervention group compared to the control group.27 The 2-minute walk test score and 10-meter walking test score considerably increased with robot-assisted gait training combined with VR compared to the control (Table II).28
Cognitive or functional outcomes
VR games significantly increased MS patients' ratings on the Modified Fatigue Impact Scale (p = 0.011) and Montreal Cognitive Assessment (p 0.001).33 The Berg Balance Scale and Phonemic Fluency Test scores were significantly higher after robot-assisted gait training mixed with VR compared to the control group.28In addition, immersive VR was successful at increasing postural stability on a hard surface with the eyes closed, right foot postural stability, and functional mobility in all situations.29
While 6-minute walk-based endurance was dramatically increased and the time to perform the Four Square Step was greatly reduced post-intervention. However, treadmill training and VR-based interventions did not significantly improve joint kinematic and kinetic characteristics.11 However, as compared to the control group, hip flexor strength, hip range of motion, and knee flexibility all increased.30 The Wii Balance Board System (WBBS) group had a reduced percentage of non-fallers and accidental falls, and more successful for static standing balance measurements and walking speed.34 The Berg Balance Score was dramatically raised by the Computer-Assisted Rehabilitation Environment system. The timed up-and-go test score, the distance walked in 25 feet, and the duration of a 6-minute walk, however, did not show any significance improvement(Table II).11
Table I: Characteristics of the included studies and participants.
|
Publication Year |
Country |
Study design & population |
Study duration |
Number of participants |
Eligibility Criteria |
Exclusion criteria |
|
Al‐Sharman et al., 201927 |
Jordan |
Observational cross‐sectional design; MS participants |
August 2016- August 2017 |
40; MS: 20; age‐ and gender‐matched controls: 20 |
a) Confirmed diagnosis of MS. b) Ability to walk independently. c) No exacerbation of symptoms<30days d) Age > 18 years e) Capacity to give informed consent f) No experience of Wii Balance Board |
a) Presence of head injury, stroke, vestibular dysfunction, or peripheral neuropathy), b) Presence of orthopaedic conditions c) Presence of severe cognitive deficits or behavioural disorders |
|
Gutierrez et al., 201328,29 |
Spain |
Prospective interventional study; MS in according to the revised McDonald criteria (2001) |
NR |
50; experimental group: 25; control: 25 |
a) Age 20-60 years; b) Confirmed diagnosis of MS. c) Medically stable < 6 months. d) Impaired balance of demyelinated lesions by MRI. e) EDSS score of 3-5. f) Hauser ambulatory index > 4. g) MMES≥24. h) No visual deficits. i) Internet connection at home. |
a) Diagnosed with another disease that affects balance. b) Relapse in the month before baseline or during the intervention process c) Received steroid cycle before beginning evaluation protocol. |
|
Leocani et al., 200712 |
Italy |
Prospective interventional study; |
NR |
24; MS patients: 12; control: 12 |
a) Patients affected MS according to Lublin criteria. |
a) Severe disability (EDSS>6.5), b) Clinical impairment of vision (FS>1; visual acuity < 7/10) c) Impairment in right upper limb motor function. |
|
Maggio et al., 202030 |
Italy |
RCT, Relapsing-remitting and secondary progressive MS, |
November 2017-November 2018 |
60; Experimental Group: 30, Control Group: 30 |
a) Confirmed diagnosis of MS. (Thompson et al., 2018); b) Stable in therapy at least < 6 months. c) Mild/moderate cognitive impairment (MoCA >18) (Ng et al., 2015); d) Absence of severe medical and psychiatric illness. e) Auditory and visual disturbances) |
a) age >75 or <18 years; b) Severe medical/psychiatric illness c) MS clinical or neuroradiological relapse in last 6 months. d) Expanded Disability Status Scale (EDSS) >7 (MeyerMoock, Feng, Maeurer, Dippel, & Kohlmann, 2014). |
|
Munari et al., 202031 |
Italy |
Single-blind, RCT; primary progressive, secondary progressive, relapsing-remitting MS |
November 2016 to November 2017 |
17; RAGT + VR group: 8, RAGT group: 9 |
a) Diagnosis of primary progressive Secondary progressive, relapsing-remitting MS b) EDSS score between 3-6. c) Mini-Mental State score > 24 d) Age > 18 years and <65 years |
a) MS relapse during the 3 months b) Psychiatric disorders drugs abuse c) Changes in MS symptoms. d) Contraindications to RAGT. e) Neurological/orthopedic conditions f) Osteoarthritis/neuropathy/joint. g) Cardiovascular co-morbidity. h) concurrent participation other studies |
|
Ozkul et al., 201932 |
Turkey |
Single-blinded RCT
|
NR |
54; Immersive virtual reality group: 17; Balance training group: 17; Control group: 17 |
a) The diagnosis of definite relapsing-remitting MS according to the revised McDonald criteria 2010 b) 18–65 years of age c) An Expanded Disability Status Scale (EDSS) score under 6 |
a) Relapses < 3 months, b) Having a disease in which exercise was contraindicated, c) Having orthopedic, vision, hearing, or perception problems |
|
Peruzzi et al., 201511 |
Italy |
A pilot study, repeated measures design; relapsing-remitting MS |
NR |
8; |
a) EDSS score 3-6; Ambulation Index 3 (mild to moderate impairment) b) Mini-mental state examination score > 24 |
a) Chronic medical illnesses, severe visual deficits, severe ataxia during gait, and major depression. b) Botulinum toxin injection within the past four months or functional surgery in the past six months. |
|
Peruzzi et al., 2016333 |
Italy |
Single-blind RCT design with assessments pre- and post-intervention |
NR |
25; control group: 11, experimental group: 14 |
a) A diagnosis of relapsing-remitting multiple sclerosis b) An expanded disability status c) Scale-EDSS score between 3 and 5.5 d) A mini-mental state examination score of 26 or above e) No relapses within the six months before the study. |
a) Chronic medical illnesses, severe visual deficits, severe ataxia, or severe depression. b) Botulinum toxin injection within the past four months or functional surgery in the past six months. c) Concurrent physical therapy for duration of the study. |
|
Prosperini et al., 201334 |
Italy |
2-period crossover pilot RCT; MS according to McDonald Revised Criteria |
24 weeks |
36; 1:1 (Experimental: Control) |
a) 18-50 years (inclusive); a relapsing/remitting/ secondary progressive MS course b) An EDSS score < 5.5 c) Ability to walk without resting for at least 100 meters d) Presence of an objective balance disturbance |
a) Relapses occurring over previous 6 months b) Initiation of disease modifying or symptomatic treatments c) Seizures, severe blurred vision, concomitant otological or vestibular diseases (non-MS related); psychiatric disorders or severe cognitive impairment; and cardiovascular and respiratory disorders. |
|
Streicher et al 201835 |
USA |
Retrospective chart review |
1 September 2013 and 1 February 2016 |
62; Traditional physical therapy (n=28), CAREN physical Therapy (N=34) |
a) Were 18 years of age or older b) Documented diagnosis of MS c) McDonald diagnostic criteria for MS d) Completed at least three physical therapy sessions e) One documented functional outcome after course of PT |
Neurological condition other than multiple sclerosis or a clinically significant orthopaedic or medical comorbidity |
Sensory outcomes
In comparison to the control, the videoconference-monitored tele rehabilitation using the Xbox 360 console was more successful at highlighting somatosensory and other sensory responses.32 When paired with VR, robot-assisted gait training significantly increased performance on the Paced Auditory Serial Addition Test in comparison to the control group(Table II).28
Table II a: Intervention characteristics and outcomes
|
Reference |
Intervention used |
Mode of application and outcome measure |
Scales or questionnaires used |
Key Outcome |
Reported limitations |
|
Al‐Sharman et al., 201927 |
Non-immersive VR system (Nintendo Wii Plus & Balance Board, large standard LCD, and its software |
Each participant was asked to perform the game for five times (blocks). Each block lasted for 2 min with total practice of 10 min. A baseline block was performed and discarded from analysis. Participants were allowed to rest between blocks if needed |
The Arabic version of the Modified Fatigue Impact Scale (MFIS); Arabic version of the Montréal Cognitive Assessment (MOCA) total score |
a) Both groups had a practice‐ related improvement in performance (p < .001, time required to complete VR game; p < .001, errors recorded) b) No significance b/w the MS & control with respect to extent of improvement in performance across blocks (VR game p=.08; errors recorded p=0.44) c) No interaction effect between block and group for both of the outcome measures (time to complete VR game, p=0.07; errors recorded, p= 0.27) d) Significant correlations b/w performance as indicated by change in number of errors and MOCA score (ρ = −0.75, p<0.001) and MFIS score (p=0.55, p=0.011). |
a) Cross‐sectional design b) Less sample size c) Only relapsing remitting MS individuals with minimal disability participated in the study d) Factors influencing motor learning such as sleep disturbances, depression, and anxiety have not been assessed |
|
Gutierrez et al., 201328,29 |
Tele rehabilitation treatment using the Xbox 360 console monitored via videoconference |
Control Pts (CG; n = 25) received physiotherapy treatment twice/week (40 min/session). Treatment was based on low-loads strength exercises (10 min/session), proprioception & gait facilitation exercises (20min/session). Muscle-tendon stretching (10 min/session). Intervention Tele-rehabilitation using Xbox 360® console. Pts attended 40 sessions, 4 sessions/week (20 min per session). |
A computerised dynamic post-urography and clinical outcomes (Berg Balance and Tinettti scales); fatigue self-perceived was taken into account with an analogue visual scale; The Sensory Organisation Test (SOT) and the Motor Control Test (MCT) were used |
a) There was a significant difference between the experimental group and treatment group with respect to Compues to-SOT (P<0.001); PREF. VISUAL (P<0.001); VESTIBULAR (P<0.001); MTC (p=0.003); BBS (P<0.001); TT (P<0.001) b) No difference between the groups with respect to VISUAL (p=0.095); SOMATOSENSORIAL (p=0.734) c) There was a significant difference between two groups with respect to CES (p=0.000); PREF (p=0.000); VEST (p=0.000); MCT (ms) (p=0.003) d) There was no difference between groups are observed in ViR (p=0.095); SR (p=0.734) |
a) Non-probabilistic sampling b) The research was not blind c) No follow-up was performed to conclude that the improvements remained stable over time d) The size of the treatment effect was not evaluated e) The VR system proposed activities were not specifically designed to serve a rehabilitative purpose
|
|
Leocani et al., 200712 |
motor-tracking task using a virtual reality object |
Individuals performed a motor-tracking task with their right upper limb, following the trajectory of an object projected on a screen along with online visual feedback on hand position from a sensor on the index finger. A pretraining test (3 trials), a training phase (12 trials), and a post training test (3 trials) were administered. |
NR |
Pre-training Performance a) Both MS and control groups were less precise in planes involving depth (vertical & horizontal) compared to frontal (controls: P=0.0002; MS:P=0.0018). b) The MS group performed worse than control participants (P=0.0056). Post-training Performance a) Both patients and control participants were significantly less precise in the depth planes compared to the frontal (controls: P = .006; MS: P = .0005). b) Compared to control participants, MS group performed significantly worse in frontal plane (P=0.015); differences were not significant in the depth planes. Post-training Improvement a) Significant difference between 2 groups was observed in depth planes, improvement in 9 (75%) control & in 4 (33.3%) MS pts (P=0.04). b) The mean improvement was significantly different from 0 in both groups and all planes (P<0.04), except in MS patients in the depth planes c) Improvement in control was slightly higher in depth planes. d) Improvement in MS patients was significantly higher in frontal plane(P=0.039). e) MS group improved less compared to control in depth planes (P=0.03). |
NR |
|
Maggio M et al., 202030 |
Semi-immersive virtual reality |
Control A traditional rehabilitation training, face-to-face approach b/w patient & therapist. Tasks were presented using a pencil-and-paper method to stimulate cognitive skills. Experimental group VR training, consisted of providing pt. with CR in the VR system, BTS-Nirvana (Figure 1). |
Control Trunk Test (CONT TK); Timed Up and Go test (TUG); Tinetti Test |
a) No significant difference was observed between the groups with respect to the CONT TK (p=0.85; Zeta=0.17) and TUG SX (p=0.13; Zeta=0.85) b) A significant improvement was observed in TUG DX (p=0.00; Zeta=0.20); TINETTI B (p=0.00; Zeta=0.56) and TINETTI G (p=0.00; Zeta=0.24)
|
NR |
|
Munari D et al., 202031 |
Robot-assisted gait training (RAGT) combined with virtual reality |
RAGT was performed on a G-EO System (Reha Technology, Olten, Switzerland). Each session lasted up to 40 minutes: 5 minutes for positioning the patient on the device, 30 minutes for RAGT, and 5 minutes for removing the patient from the device. The body weight support protocol was gradually set to 2 weeks at 30% 186 of body weight, 2 weeks at 20%, and 2 weeks at 10%. The RAGT + VR group underwent training on the same device (GE-O System) engendered by non-immersive VR. |
The Paced Auditory Serial Addition Task (PASAT), The 2-Minutes Walk Test (2MWT), The Phonemic Fluency Test (PFT), The Novel Task, The Digit Symbol (DSymb), The Multiple Sclerosis Quality Of Life-54 (MSQOL-54), The 10-Meter Walking Test (10MWT), The Berg Balance Scale (BBS),Gait analysis and Stabilometric assessment. |
a) Group comparison showed a significant change on 2MWT (p = 0.023; Z: –2.269) b) No significant post-training effects were observed for RAGT group c) Significant improvement in the PASAT score for the RAGT + VR group after treatment (p = 0.012; Z: –2.521) and on the 2MWT (p = 0.012; Z: – 2.524) Secondary Outcomes a) Significant post-treatment improvement for the RAGT group were found in the MSQOL-54 MHC (p = 0.018; Z:– 2.375), MSQOL-54 PHC (p = 0.017; Z:–2.384), 10MWT (p = 0.018; Z:–2.371), and BBS (p = 0.016; Z:–2.414) b) Group comparison showed significant improvement on PFT (p = 0.012; Z:–2.521) and the NT-IR after treatment (p = 0.012; Z:–2.521) 402 and at follow-up (p = 0.012; Z:–2.521; p = 0.012; Z:–2.521) for the RAGT + VR group. c) Significant improvements were found in the MSQOL-54 PHC composite (p = 0.017; Z:–2.384) and the MSQOL-54 MHC composite (p = 0.018; Z:–2.371). d) Significant changes were found on 10MWT (p = 0.012; Z:–2.251) and the BBS (p = 0.011; Z:–2.539) after treatment. |
a) The sample size is small. b) Fully immersive VR may provide a complete simulated experience through the support of multiple sensory output devices to enhance stereoscopic view of the environment through movement of the user’s head, as well as audio and haptic devices. c) The lack of a follow-up assessment at 3 or more months after training is needed to further assess the persistence of the training effect |
Quality of life
The Multiple Sclerosis Quality of Life-54 was used to measure participants' quality of life, and the combination of robot-assisted gait training and VR considerably improved it compared to the control group.28 When compared to the control, immersive VR considerably reduced the severity of weariness (Table II).29
Table II b: Intervention characteristics and outcomes
|
Reference |
Intervention used |
Mode of application and outcome measure |
Scales or questionnaires used |
Key Outcome |
Reported limitations |
|
Ozkul et al., 201932 |
Immersive virtual reality, Balance training group |
Exercise training started with Pilates based core stability training in both IVRG and BTG. Pilates training took about 30 min. After Pilates, 10 min of rest and then 20 min of IVR or balance training (BT) were applied in each session. The RAGU (Augmented Reality Applications in Rehabilitation) was used for the IVR System study. The system (RAGU) included two games for improving balance (Fig. 6). |
The Berg Balance Scale (BBS) and posturography (Biodex Balance System-BioSwayTM), Timed Up and Go (TUG) Test, Fatigue Severity Scale (FSS), |
a) Balance: Postural stability on eyes closed-firm surface condition was significantly larger in the IVRG than in the CGv. Improvements of postural stability on the right foot were significantly larger in both training groups than CG (p < 0.0001 between IVRG and CG, p < 0.0001 between the BTG and CG). b) Functional mobility: Functional mobility under all conditions were significantly greater in both training groups than the CG (p < 0.0001 between the IVRG and CG, p < 0.0001 between the BTG and CG). c) Fatigue: Post hoc tests with Bonferroni correction indicated that decrements of fatigue severity in both training groups were significantly larger than the CG (p < 0.0001 between the IVRG and CG, p < 0.0001 between the BTG and CG). |
a) Its sample size is small and thus, has low statistical power. b) The follow-up was not performed, so we could not comment on the permanence of the effects. c) there was not a group that received only Pilates training. d) We did not investigate the effects of VR on the activities of daily living in MS patients. |
|
Peruzzi A et al., 2015 11 |
Trade mill training and VR-based intervention |
The participants walked on the TM while watching a VR environment representing a tree lined trail. Subjects were required to pass obstacles (puddles and logs) appearing on the trail. Subjects were asked to walk overground in the gait analysis laboratory under two conditions: a) at comfortable speed (single task and dual task condition). |
The six-minute walk test (6MWT) was used to assess walking endurance. The Four-Square Step Test (FSST), a timed test consisting of stepping over an obstacle was used to evaluate obstacle negotiation, The EDSS was assessed at each evaluation session by the same physician. |
Joint kinematics and kinetics: Joint kinematic and kinetic parameters during ST did not show significant changes in the most affected side. In DT, the maximum value of hip extension at terminal stance in the most affected side showed an increase, although not significant, between Pre and F-Up (Pre: 14.5 ± 5.1 deg, F-Up: 18.2 ± 5.4 deg; p = 0.07). The maximum ankle plantar-flexion during the pre-swing phase increased in the least affected side (Pre: 6.4 ± 6.9 deg, Post: 12.6 ± 7.2 deg, F-Up: 11.8 ± 7.2 deg; p = 0.07). Performance and impairment -based measures: The distance walked during the 6MWT tended to increase by 8% at Post and by 23% at FUp, which reflects improved endurance. Time to execute the FSST significantly decreased by 22% at Post (p=0.02) & 37% at F-Up (p=0.02). |
The sample size was limited. This was an open label pilot study |
|
Peruzzi A et al., 201733 |
VR based treadmill training vs treadmill training |
Control group: A treadmill-based rehabilitation programs; Experimental group: a six-weeks VR based treadmill training and a six-weeks treadmill training program on gait measures of Persons with MS. To evaluate the effects of the training, a gait analysis was performed pre and post intervention under single and dual task conditions. |
The six-minute walk test (6Mwt) [27] and the 10mwt were used to assess walking endurance and speed, respectively; the timed up and go (TUG) [28] was used to assess mobility and the Berg balance scale (Berg) [29] was used to assess balance; the four square step test – (FSST)[30], a timed test consisting of stepping over an obstacle, was used to evaluate obstacle negotiation [16,31]. Disability was assessed using the EDSS. |
a) Both the experimental and control group significantly improved gait speed, cadence & stride length in ST & DT. b) A trend towards larger stride length was observed in VR-TT vs TT group post training in ST and DT. c) Experimental group also showed a significant increase of the knee and hiprange of motion of the MA side in ST, and of the hip range of motion of the MA side in DT. d) Significant greater improvements were observed in the VR-TT group post training in the hip flexor power in the MA side in both ST (B: -(0).797, CI95%: [-1.319-0.276], p¼0.004) and DT conditions (B: -0.603, CI 95%: [-1.028– -0.179], p¼0.007). |
a) This is a small feasibility b) study with a fairly reduced sample size. c) The groups were not matched at baseline, therefore, some of the improvements or lacks may need to be taken with caution. d) We did not include measures to explore specific changes in cognitive function, which may allow for further understanding of the changes due to the motor-cognitive interference training |
|
Prosperini L et al., 201334 |
Group A: 12-week period of home-based Wii Balance Board System (intervention), followed by 12-week (observation) Group B: patients were given the treatment period in reverse order.
|
During the 12-week active period, each patient was submitted to daily sessions (with the exception of the weekend) of home-based training with WBBS, each lasting 30 minutes.
|
Primary endpoint was mean difference in static standing balance measures (ie, COP path) at T1 and T2 visits, as compared with baseline (T0) evaluation. Secondary endpoints were the mean differences in clinical scales (FSST and 25-FWT) and in self- administered questionnaire (MSIS-29) at T1 and T2 visits, as compared with to baseline (T0) evaluation. |
a) The simple contrast analyses revealed that WBSS training was effective in all endpoints, regardless of the order of treatment. b) In group A, there was a significant improvement in COP path, FSST, and MSIS-29 at the end of intervention period and a trend toward a return to baseline values at the end of the observation period. c) A residual effect on primary endpoint was found in group A even at the end of the observation period. d) In group B the improvement in walking speed after WBBS training reached statistical significance (P < .05) e) At the end of the 24-week study period, there was a proportion of non-fallers (n = 17, 50%) greater than that one (n = 12, 35%) relative to the 12 weeks before the study entry (P = .048 by the McNemar–Bowker test). No accidental falls were reported by patients while performing WBBS training. |
a) The small sample size, absence of blindness, and the study design lacking a washout period. b) Data regarding the occurrence of accidental falls prior to study enrolment were not reliably captured, therefore affecting a consistent comparison with respect to study period c) Lower extremity strength was not measured; hence, we cannot assess whether muscle reinforcement may have played a role in determining the balance improvement. d) Last, an evaluation of sitting balance performance is lacking,
|
|
Streicher et al 201854 |
Computer Assisted Rehabilitation Environment system |
Physical therapy sessions lasted approximately 60 minutes regardless of the setting. Traditional physical therapy in a gym consisted of stretching, balance and gait training, and strengthening exercises. During exercise on the CAREN system, four applications were commonly used for gait and balance training (Figure 2), occasionally with additional gait or balance exercises |
Berg Balance Scale (BBS): To test standing balance; Timed 25-Foot Walk (T25FW): To measure of maximum gait velocity on a short distance; Timed Up and Go test (TUG): To measure dynamic balance in which an individual stands up from a chair, walks 3 meters, then turns around and walks back to the chair and sits down. The individual is timed from the moment their pelvis lifts off the chair until their pelvis reaches the chair again when sitting down; and 6-Minute Walk Test (6MWT): To measure both gait velocity and endurance, where the total distance walked in 6 minutes is measured. The 6MWT is able to discriminate between healthy individuals and those with multiple sclerosis |
a) There was a statistically significant improvement on the BBS between baseline and at the end of treatment, both for patients who received traditional PT (n=25, P<0.001, d=0.41), and for patients who received PT in CAREN system. (n=31, P<0.001, d=0.44). b) The TUG task showed minimal change after traditional physical therapy (n=28, P=0.98, d=0.055), while CAREN users had a significant improvement (n=33, P=0.0021, d=0.29). c) The within-group difference on the T25FW was not statistically significant after traditional PT (n=27, P=0.42, d=0.001), while there was a statistically significant improvement after CAREN PT compared to baseline (n=33, p=0.0048, d=0.28). d) There was slight decrease in performance in the 6MWT after traditional physical therapy (n=12, P=0.74, d=0.038). CAREN users showed significant improvement (n=18, P=0.0012, d=0.34). |
a) Randomization was not possible due to it was a retrospective chart review. b) Baseline differences between the CAREN group and the traditional physical therapy group at baseline exceeded the reported minimum clinically importance difference values for both the T25FW and the 6MWT, in favor of the CAREN group, although the P values do not reach statistical significance. c) Dosing’ of the physical therapy interventions favored the CAREN user group over the traditional therapy group |
DISCUSSION
Techniques for virtual neuro-rehabilitation for MS patients are currently gaining popularity.35,36VR programs are being used more frequently in rehabilitation facilities to enhance motor skills.8There is discrepancy on how to employ VR in a domestic environment and no standard protocol for neuro-rehabilitation are available. There is argument that the use of TR can be efficient, effective, and increases the compliance of therapy. Compliance can be easily observed, with regular video conferences to provide immediate feedback. Most researchers recommend that when using tele-rehabilitation with VR in a home-based setting, treatment plans can be observed by at least one caregiver for safety concerns.36,37 Also, it is important to remember that during the tele-rehabilitation process, suitable and accurate instructions for timely compensatory corrections should be considered.
Recently the non-pharmacological approaches has been brought to light by the ineffectiveness or due to the subpar efficacy of pharmaceutical treatments for cognitive and motor deficits in the rehabilitation of patients with MS or similar diseases.38Evidence from the literature suggests that virtual gaming methods are useful for reducing social disadvantages and enhancing MS-related limitations.37-39A flourishing exercise training business is being driven by a variety of VR technologies, including cellphones, personal computers, commercial systems (such the Nintendo Wii, Xbox 360, and Home balance), custom-designed devices, or modified video games. TheseVR equipments will enhance Patients' engagement, activity levels, energy, and sense of well-being in the home environment.32,34,37MS patients can themselves train their motor abilities and engage with others by using virtual gaming approaches.40Other neurological problems such as cerebral palsy,41 Parkinson disease42-44,autism44,45, Down’s syndrome, 46,47 and stroke48,49 can also be managed using virtual gaming strategies. Consequently, neuro-rehabilitation programs are among the most well-liked treatments for minimizing MS-related disability with lesssocial drawbacks. This systematic review imply that VR has extra advantages for cognitive and motor rehabilitation, particularly when used in conjunction with other treatments.
Most studies included individuals provided they met the updated McDonald and Lublin criteria for MS diagnosis and had an EDSS score of less than 5. This means that the MS diagnosis is based on the McDonald criteria and Lublin criteria.50 Similar findings were found by Massetti et al. after conducting a systematic review.8,51Due to the fact that most of the included research were from Italy, VR approaches received more attention there.
The included studies employed a variety of VR approaches, including semi-immersive, tele-rehabilitation, immersive, and immersive techniques (Table II).33In two trials, 11,30 where conventional treadmill training served as the control group, the VR-based treadmill training was compared. The superiority of the VR-based treadmill training was demonstrated in an RCT with a bigger sample by Peruzzi et al.30 In addition to increasing hip flexor power and knee/hip range of motion, the VR treadmill technique also resulted in a longer stride length in the VR group.11
The review found that the robot-assisted gait training and the motor-tracking task employing a VR object were the most effective methods for enhancing motor abilities in videoconference-monitored tele-rehabilitation using the Xbox 360 console.27,32 Also, the VR method group saw improvements in their scores on the Montreal Cognitive Assessment, Berg Balancing Scale, Modified Fatigue Impact Scale, and Phonemic Fluency Test.8,23The VR-based rehabilitation strategies were successful in improving the MS patients' quality of life, however only one study assessed this. The patients' higher quality of life implied that their social interactions and routine activities had improved.39Contrarily, the gaming VR method was reportedto be ineffectual in one of the studies.33 In general, our results agreed with those of Massetti et al. where there is trend towards improvement and beneficial outcome in terms of compliance and social acceptability. In conclusion, VR-based neuro-rehabilitation improved the motor and cognitive results in MS patients.51 Virtual reality (VR) has been proposed as a potential substitute for conventional motor rehabilitation regimens.
Future research perspective
There is need to standardize the protocol of VR in MS patients by conducting larger multi-centric RCTs. Moreover, there was no standard method of reporting the findings, and comparison with existing pharmaceutical treatments is required. Furthermore, most of the studies are from developed countries due to the reason of high cost of the VR and affordability issue needs to be addressed for low and middle-income countries and RCTs needs to be conducted in underdeveloped countries as well. There is need to compare VR approaches on a single platform and provide data that will help doctors and physical therapists improve patient outcomes.The clinical outcomes may be influenced by VR technology or immersion degree, although this is uncertain. To confirm these findings, further investigation is necessary.
CONCLUSION
Rehabilitation using cutting-edge VR tools could improve MS patients' outcomes by enhancing lower limb function and learning along with the quality of life. In addition, it increases motivation and involvement of MS patients byenhancing their receptivity to therapy. Homebased therapy is cost/time effective and convenient for both patient and the rehabilitation team.
ACKNOWLEDGEMENTS
I thank the Dr.Manal Matouq Abdulrahman for her expertise and assistance throughout all aspects of this study and for her voluble help during the data extraction process of the study.
CONFLICT OF INTEREST
None of the authors / co-authors have any conflict of interest to declare.
FUNDING
None.
REFERENCES
1. Walton C, King R, Rechtman L, Kaye W, Leray E, Marrie RA, et al. Rising prevalence of multiple sclerosis worldwide: Insights from the Atlas of MS. Mult Scler J 2020;26(14):1816-21.https://doi.org/10.1177/1352458520970841
2. Benedetti MG, Piperno R, Simoncini L, Bonato P, Tonini A, Giannini S. Gait abnormalities in minimally impaired multiple sclerosis patients. Mult Scler J 1999;(5):363-8. https://doi:10.1177/135245859900500510
3. Filli L, Sutter T, Easthope CS, Killeen T, Meyer C, Reuter K, et al. Profiling walking dysfunction in multiple sclerosis: characterisation, classification and progression over time. Sci Rep 2018;8(1):4984.https://doi.org/10.1038/s41598-018-22676-0
4. Jongen PJ, Ter Horst AT, Brands A. Cognitive impairment in multiple sclerosis. Minerva Med 2012;103(2):73-96.
5. Milo R, Miller A. Revised diagnostic criteria of multiple sclerosis. Autoimmun Rev 2014;13(4-5):518-24. https://doi:10.1016/j.autrev.2014.01.012
6. Physiopedia. Virtual Reality Treatment for Multiple Sclerosis. [Accessed on: July 1, 2022]. Available from URL: https://www.physio-pedia.com/Virtual_Reality_Treatment_for_Multiple_Sclerosis
7. Kim A, Schweighofer N, Finely JM. Locomotor skill acquisition in virtual reality shows sustained transfer to the real world. J NeuroEng Rehabil 2019;16(1):113. https://doi.org/10.1186/s12984-019-0584-y
8. Massetti T, Trevizan IL, Arab C, Favero FM, Ribeiro-Papa DC, de Mello Monteiro CB. Virtual reality in multiple sclerosis–a systematic review. Mult Scler Relat Disord 2016;8:107-12.https://doi:10.1016/j.msard.2016.05.014
9. Straudi S, Basaglia N. Neuroplasticity-Based Technologies and Interventions for Restoring Motor Functions in Multiple Sclerosis. Adv Exp Med Biol 2017;958:171-85. https://doi.org/10.1007/978-3-319-47861-6_11
10. Shalabi K. Neuroscience of motor learning in adults with non-dominant hand. J Crit Rev 2020;7(6):27-30.https://doi.org/10.31838/jcr.07.06.07
11. Peruzzi A, CereattiA, Della Croce U, Mirelman A. Effects of a virtual reality and treadmill training on gait of subjects with multiple sclerosis: a pilot study. Mult Scler Relat Disord2016;5:91-6. https://doi.org/10.1016/j.msard.2015.11.002
12. Leocani L, Comi E, Annovazzi P, Rovaris M, Rossi P, Cursi M,et al. Impaired short-term motor learning in multiple sclerosis: evidence from virtual reality. Neurorehabil Neural Repair 2007;21(3):273-8.https://doi.org/10.1177/1545968306294913
13. Baram Y, Miller A. Virtual reality cues for improvement of gait in patients with multiple sclerosis. Neurology 2006;66(2):178-81.https://doi.org/10.1212/01.wnl.0000194255.82542.6b
14. Cattaneo D, Ferrarin M, Frasson W, Casiraghi A. Head control: volitional aspects of rehabilitation training in patients with multiple sclerosis compared with healthy subjects. Arch Phys Med Rehabil 2005;86(7):1381-8. https://doi.org/10.1016/j.apmr.2004.12.029
15. Casadio M, Sanguineti V, Morasso P, Solaro C. Abnormal sensorimotor control, but intact force field adaptation, in multiple sclerosis subjects with no clinical disability. Mult Scler J 2008;14(3):330-42. https://doi.org/10.1177/1352458507085068
16. Graziadio S, Davison R, Shalabi K, Sahota KMA, Ushaw G, Morgan G, et al. Bespoke video games to provide early response markers to identify the optimal strategies for maximizing rehabilitation. Proceedings of the 29thAnnual ACM Symposium on Applied Computing. 2014 March 24. https://doi.org/10.1145/2554850.2554953
17. Peñasco-Martín B, de los Reyes-Guzmán A, Gil-Agudo Á, Bernal-Sahún A, Pérez-Aguilar B, de la Peña-González AI.Aplicación de la realidad virtual en los aspectos motores de la neurorrehabilitación [Application of virtual reality in the motor aspects of neurorehabilitation]. Rev Neurol2010;51(8):481-8.https://doi.org/10.33588/rn.5108.2009665
18. Davison R, Graziadio S, Shalabi K, Ushaw G, Morgan G, Eyre J. Early response markers from video games for rehabilitation strategies. ACM SIGAPP App Comput Rev 2014;14(3):36-43. http://dx.doi.org/10.1145/2670967.2670970
19. de Rooij IJ, van de Port IG, Meijer JG. Effect of Virtual Reality Training on Balance and Gait Ability in Patients With Stroke: Systematic Review and Meta-Analysis. Phys Ther 2016;96(12):1905-18. https://doi.org/10.2522/ptj.20160054
20. Iruthayarajah J, McIntyre A, Cotoi A, Macaluso S, Teasell R. The use of virtual reality for balance among individuals with chronic stroke: a systematic review and meta-analysis. Top Stroke Rehabil2017;24(1):68-79. http://doi.org/10.1080/10749357.2016.1192361
21. Li Z, Han XG, Sheng J, Ma SJ. Virtual reality for improving balance in patients after stroke: A systematic review and meta-analysis. Clin Rehabil 2016;30(5):432-40. https://doi.org/10.1177/0269215515593611
22. Harris DM, Rantalainen T, Muthalib M, Johnson L, Teo WP. Exergaming as a Viable Therapeutic Tool to Improve Static and Dynamic Balance among Older Adults and People with Idiopathic Parkinson's Disease: A Systematic Review and Meta-Analysis. Front Aging Neurosci 2015;7:167. https://doi.org/10.3389/fnagi.2015.00167
23. Donath L, Rössler R, Faude O. Effects of Virtual Reality Training (Exergaming) Compared to Alternative Exercise Training and Passive Control on Standing Balance and Functional Mobility in Healthy Community-Dwelling Seniors: A Meta-Analytical Review. Sports Med 2016;46(9):1293-309. https://doi.org/10.1007/s40279-016-0485-1
24. Molina KI, Ricci NA, de Moraes SA, Perracini MR. Virtual reality using games for improving physical functioning in older adults: a systematic review. J Neuroeng Rehabil 2014;11:156. https://doi.org/10.1186/1743-0003-11-156
25. Booth V, Masud T, Connell L, Bath-Hextall F. The effectiveness of virtual reality interventions in improving balance in adults with impaired balance compared with standard or no treatment: a systematic review and meta-analysis. Clin Rehabil 2014;28(5):419-31. https://doi.org/10.1177/0269215513509389
26. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8(5):336-41. https://doi.org/10.1016/j.ijsu.2010.02.007
27. Maggio MG, De Luca R, Manuli A, Buda A, Foti Cuzzola M, Leonardi S, et al. Do patients with multiple sclerosis benefit from semi-immersive virtual reality? A randomized clinical trial on cognitive and motor outcomes. Appl Neuropsychol Adult 2022;29(1):59-65. https://doi.org/10.1080/23279095.2019.1708364
28. Munari D, Fonte C, Varalta V, Battistuzzi E, Cassini S, Montagnoli AP, et al. Effects of robot-assisted gait training combined with virtual reality on motor and cognitive functions in patients with multiple sclerosis: A pilot, single-blind, randomized controlled trial. Restor Neurol Neurosci 2020;38(2):151-64. https://doi.org/10.3233/RNN-190974
29. Ozkul C, Guclu-Gunduz A, Yazici G, Atalay Guzel N, Irkec C. Effect of immersive virtual reality on balance, mobility, and fatigue in patients with multiple sclerosis: A single-blinded randomized controlled trial. Eur J Integr Med 2020;35:101092. https://doi.org/10.1016/j.eujim.2020.101092
30. Peruzzi A, Zarbo IR, Cereatti A, Della Croce U, Mirelman A. An innovative training program based on virtual reality and treadmill: effects on gait of persons with multiple sclerosis. Disabil Rehabil 2017;39(15):1557-63. https://doi.org/10.1080/09638288.2016.1224935
31. Prosperini L, Fortuna D, Giannì C, Leonardi L, Marchetti MR, Pozzilli C. Home-based balance training using the Wii balance board: a randomized, crossover pilot study in multiple sclerosis. Neurorehabil Neural Repair 2013;27(6):516-25. https://doi.org/10.1177/1545968313478484
32. Gutiérrez RO, Galán Del Río F, Cano de la Cuerda R, Alguacil Diego IM, González RA, Page JC. A telerehabilitation program by virtual reality-video games improves balance and postural control in multiple sclerosis patients. NeuroRehabilitation. 2013;33(4):545-54.https://doi.org/10.3233/nre-130995
33. Al-Sharman A, Khalil H, El-Salem K, Alghwiri AA, Khazaaleh S, Khraim M. Motor performance improvement through virtual reality task is related to fatigue and cognition in people with multiple sclerosis. Physiother Res Int 2019;24(4):e1782. https://doi.org/10.1002/pri.1782
34. Streicher MC, Alberts JL, Sutliff MH, Bethoux F. Effects and feasibility of virtual reality system vs traditional physical therapy training in multiple sclerosis patients. Int J Ther Rehabil 2018;25(10):522-8. https://doi.org/10.12968/ijtr.2018.25.10.522
35. Ortiz-Gutiérrez R, Cano-de-la-Cuerda R, Galán-del-Río F, Alguacil-Diego I, Palacios-Ceña D, Miangolarra-Page J. A Telerehabilitation Program Improves Postural Control in Multiple Sclerosis Patients: A Spanish Preliminary Study. Int J Environ Res Public Health 2013;(11):5697-710. https://doi.org/10.3390/ijerph10115697
36. Mahajan HP, Spaeth DM, Dicianno BE, Brown K, Cooper RA. Preliminary evaluation of variable compliance joystick for people with multiple sclerosis. J RehabilRes Develop 2014;(6):951-62. https://doi:10.1682/jrrd.2013.01.0023
37. Lin KH, Chen CH, Chen YY, Huang WT, Lai JS, Yu SM, et al. Bidirectional and multi-user telerehabilitation system: clinical effect on balance, functional activity, and satisfaction in patients with chronic stroke living in long-term care facilities. Sensors 2014;14(7):12451-66. https://doi.org/10.3390/s140712451
38. Amatya B, Khan F, Galea M. Rehabilitation for people with multiple sclerosis: an overview of Cochrane Reviews. Cochrane Database Sys Rev 2019;1(1):CD012732.https://doi.org/10.1002/14651858.cd012732.pub2
39. Khan F, Amatya B. Rehabilitation in Multiple Sclerosis: A Systematic Review of Systematic Reviews. Arch Phys Med Rehabil 2017;98(2):353-67. https://doi.org/10.1016/j.apmr.2016.04.016
40. Lozano-Quilis JA, Gil-Gómez H, Gil-Gómez JA, Albiol-Pérez S, Palacios-Navarro G, Fardoun HM, et al. Virtual Rehabilitation for Multiple Sclerosis Using a Kinect-Based System: Randomized Controlled Trial. JMIR Serious Games 2014;2(2):e12. https://doi.org/10.2196/games.2933
41. de Mello Monteiro CB, Massetti T, da Silva TD, van der Kamp J, de Abreu LC, Leone C, et al. Transfer of motor learning from virtual to natural environments in individuals with cerebral palsy. Res Dev Disabil 2014;35(10):2430-37. https://doi.org/10.1016/j.ridd.2014.06.006
42. Baram, Y, Aharon-Peretz J, Simionovici Y, Ron L. Walking on Virtual Tiles. Neural Processing Letters 2002;16:227-33. https://doi.org/10.1023/A:1021778608344
43. dos Santos Mendes FA, Pompeu JE, Modenesi Lobo A, Guedes da Silva K, Oliveira Tde P, Peterson Zomignani A, et al. Motor learning, retention and transfer after virtual-reality-based training in Parkinson’s disease – effect of motor and cognitive demands of games: a longitudinal, controlled clinical study. Physiotherapy 2012;98(3):217-23. https://doi.org/10.1016/j.physio.2012.06.001
44. Pompeu JE, Mendes FA, Silva KG, Lobo AM, Oliveira Tde P, Zomignani AP,et al. Effect of Nintendo WiiTM-based motor and cognitive training on activities of daily living in patients with Parkinson’s disease: A randomised clinical trial. Physiotherapy 2012;98(3):196-204. https://doi.org/10.1016/j.physio.2012.06.004
45. Kandalaft MR, Didehbani N, Krawczyk DC, Allen TT, Chapman SB. Virtual Reality Social Cognition Training for Young Adults with High-Functioning Autism. J Autism Dev Disord 2012;43(1):34-44. https://doi.org/10.1007/s10803-012-1544-6
46. Mitchell P, Parsons S, Leonard A. Using Virtual Environments for Teaching Social Understanding to 6 Adolescents with Autistic Spectrum Disorders. J Autism Dev Disord 2006;37(3):589-600. https://doi.org/10.1007/s10803-006-0189-8
47. Berg P, Becker T, Martian A, Danielle PK, Wingen J. Motor Control Outcomes Following Nintendo Wii Use by a Child With Down Syndrome. Pediatr Phys Ther 2012;24(1):78-84. https://doi.org/10.1097/pep.0b013e31823e05e6
48. Courbois Y, Farran EK, Lemahieu A, Blades M, Mengue-Topio H, Sockeel P. Wayfinding behaviour in Down syndrome: A study with virtual environments. Res Dev Disabil 2013;34(5):1825-31. https://doi.org/10.1016/j.ridd.2013.02.023
49. Baram Y, Miller A. Glide-symmetric locomotion reinforcement in patients with multiple sclerosis by visual feedback. Disabil Rehabil Assist Technol 2010;5(5):323-6. https://doi.org/10.3109/17483101003671717
50. Doud AJ, Cassady K, Grande A, He B. A thought-controlled immersive virtual reality platform for motor learning applied with cortical and basal ganglia stroke survivors. Circulation 2013;128(suppl_22):Abstract18886.
51. Halder S. Application of Virtual Reality in Cognitive Rehabilitation: A Road Ahead. In: Emerging Advancements for Virtual and Augmented Reality in Healthcare. IGI Global;Pennsylvania (USA) 2022. pp. 217-32. http://dx.doi.org/10.4018/978-1-7998-8371-5.ch013
|
Following author have made substantial contributions to the manuscript as under:
KMS: Concept and study design, acquisition, analysis and interpretation of data, drafting the manuscript, critical review, approval of the final version to be published
Author agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Author declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work.
GRANT SUPPORT AND FINANCIAL DISCLOSURE Author declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |