![]() https://doi.org/10.35845/kmuj.2024.23291 ORIGINAL ARTICLE
https://doi.org/10.35845/kmuj.2024.23291 ORIGINAL ARTICLE
Diagnostic accuracy of computed tomography scan against surgical indings in small bowel obstruction cases
|
1: Radiology Department, Dow University of Health Sciences/ Dr Ruth K.M. Pfau Civil Hospital Karachi, Pakistan
Email
Contact #: +92-333- 3256715 Date Submitted: December 22, 2022 Date Revised: November 21, 2023 Date Accepted: January 27, 2024 |
|
|
|
THIS ARTICLE MAY BE CITED AS: Gohar F, Sohail S, Shaikh R. Diagnostic accuracy of computed tomography scan against surgical findings in small bowel obstruction cases. Khyber Med Univ J 2024;16(1):61-6. https://doi.org/10.35845/kmuj.2024.23291 |
ABSTRACT
OBJECTIVE: To determine the diagnostic accuracy of computed tomography (CT) scan in small bowel obstruction (SBO), utilizing operative findings as the gold standard.
METHODS: This descriptive cross-sectional study was conducted at Dr. Ruth K.M. Pfau Civil Hospital Karachi, Pakistan from September 2019 to August 2020. A comprehensive assessment, including plain and contrast-enhanced CT scans of the abdomen, was performed on 267 patients with clinically suspected acute SBO. Operative findings were compared with CT results to determine diagnostic accuracy. Sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and overall diagnostic accuracy were evaluated, considering operative findings as the gold standard.
RESULTS: Out of 267 patients, 162 (60.7%) were males, and 105 (39.3%) were females, with a mean age of 33.03±10.58 years. The mean duration of symptoms was 12.11±4.13 days. Overall sensitivity, specificity, PPV, NPV, and diagnostic accuracy of the CT scan were 92.2%, 87.8%, 87.4%, 92.4%, and 89.9%, respectively. Common CT findings included dilated small bowel loops (128 cases, 100%), the point of transition (105 cases, 82%), and bowel wall thickening (71 cases, 55.5%). Post-operative analysis revealed 118 out of 128 confirmed cases and 17 additional cases initially missed by CT. Tuberculosis emerged as the leading histopathological cause (25.9%), followed by obstructed/strangulated hernias (22.2%) and adhesions (17.7%).
CONCLUSION: This study emphasizes the superior diagnostic precision of CT scans in determining the level and cause of SBO, reflecting a high sensitivity (92.2%) and specificity (87.8%). Common CT findings, including dilated bowel loops, contribute to precise identification, guiding effective clinical management.
KEYWORDS: Diagnostic Accuracy (Non-MeSH); Diagnostic Imaging (MeSH); CT scan (Non-MeSH); Histopathology (Non-MeSH); Small Bowel Obstruction (Non-MeSH); Intestinal Obstruction (MeSH); Tuberculosis (MeSH).
INTRODUCTION
Intestinal obstruction is a globally prevalent emergency condition that requires timely and accurate diagnosis to prevent morbidity and mortality. Approximately 60–85% of intestinal obstruction cases are attributed to small bowel obstruction (SBO).1,2 There are many causes of mechanical SBO like adhesions, abdominal hernias, tuberculosis and intestinal neoplasms, etc. In developed countries, adhesions are the most common cause of mechanical SBO, followed by abdominal hernias;3,4 while in developing countries, adhesions followed by intestinal tuberculosis are the most common causes of SBO.3 Adhesions can arise from various sources, including post-surgical procedures or post-inflammatory responses triggered by prior infections, radiotherapy, or chronic inflammation. These conditions can lead to peritoneal injury and initiate an inflammatory process characterized by fibrin deposition, ultimately resulting in SBO. Among these, post-surgical adhesions are common, which can occur as early as three days to two weeks.1 Intestinal tuberculosis predominantly affects the terminal ileum and cecum, regions rich in lymphoid tissue, where physiological stasis and reduced digestive activity create conditions conducive to its development. Bowel obstruction is the most common complication of intestinal tuberculosis, either due to luminal narrowing, strictures, or adhesions.5 The study done by Mubarak et al.,6 found tuberculous stricture in the majority of cases (35.8%), followed by adhesions (26.0%) and hernia (18.5%). Intestinal obstruction, especially SBO, is more common in Pakistan, Africa, and tropical countries than in other western countries.7 The mortality of SBO depends on whether complications like bowel ischemia develop or not. It may be as high as 25% for patients with complicated bowel ischemia and up to 8% for non-complicated obstruction.8 SBO needs emergency surgery if there is an absence of gas or fluid in distal intestinal segments and/or signs of bowel ischemia or perforations.6,8
While conventional radiography is the initial imaging modality for suspected SBO due to its cost-effectiveness and accessibility, its diagnostic accuracy ranges from 46-80%.1,5 Advancements in imaging, especially Computed Tomography (CT) scans, have revolutionized SBO diagnosis by not only confirming the obstruction but also detailing its cause, level, and site. The multiplanar reformatting capabilities of CT scans play a pivotal role in evaluating potential complications associated with SBO. 8-10 Contrast-enhanced CT (CECT) abdomen further clarifies the pathology of the bowel wall, mesentery, vessels, and peritoneal cavity.
Despite the potential benefits of CT scans in swiftly initiating management for SBO by providing crucial information for surgical decisions and avoiding unnecessary emergency laparotomies, their utilization remains limited in resource-constrained tertiary care hospitals. This underutilization underscores the need for evidence establishment at local level, particularly in regions where patients from rural areas are frequently referred. SBO, while potentially fatal, is a curable condition when diagnosed promptly, considering the cause, degree, and precise site of obstruction. Addressing the disparity between the acknowledged benefits of CT scans and their actual integration into healthcare facilities grappling with resource limitations is a significant challenge. The objective of this study was to ascertain the diagnostic accuracy of CT scans in SBO, using operative findings as the gold standard. This would facilitate effective surgical or medical management, playing a crucial role in averting the onset of potential complications such as bowel ischemia and perforation.
METHODS
This cross-sectional descriptive study was conducted in Radiology Department, Dr. Ruth K. M. Pfau Civil Hospital, Karachi (DUHS) from September 2019 to August 2020. Sample size was calculated by taking expected sensitivity 92% and specificity 93% of contrast enhanced CT Scan in diagnosing SBO.8 Prevalence of 21.8 %,7 desired precision of 7% and confidence interval of 95%. The estimated sample size was 267. Patients were enrolled using a non-probability sampling technique, and written informed consent was acquired from each participant. The study received approval from the Institutional Review Board under Reference # IRB-1670/DUHS/Approval/2020/117, dated July 30, 2020.
The inclusion criteria comprised individuals of any gender aged between 18 and 50 years exhibiting clinical suspicion of acute SBO, characterized by symptoms such as abdominal pain, vomiting, and an inability to pass flatus. Exclusion criteria encompassed patients allergic to intravenous contrast agents, those with impaired renal function indicated by a serum creatinine level exceeding 2 mg/dl, individuals who had undergone recent abdominal surgery, or those experiencing paralytic ileus. Additionally, participants who had undergone surgery before undergoing a CT scan were excluded from the study.
Data collection was conducted prospectively, encompassing the recording of patient demographics, including age and gender, in addition to clinical features. CT scan of the abdomen was performed before and after intravenous non-ionic contrast administration on 16 Slice Toshiba Activion Scanner in the portal venous phase (70 seconds) acquisition. The scanning parameters were 120 KV, 150 mA, 1mm collimation and 3mm slice thickness. Images were obtained in contagious axial sections from the level of the xiphisternum to pubic symphysis and reformatted in sagittal and coronal planes. No oral contrast was given. CT findings were analyzed in terms of diameter of small bowel, wall thickness, small bowel wall enhancement, presence of sudden or gradual change in luminal diameter of bowel, obstructive lesion at or around the site of obstruction, small bowel feces sign and beak sign; these findings were recorded on the proforma. Small bowel loop was labeled as dilated (diameter more than 2.5 cm measured from outer to outer wall) or collapsed (lumen barely visualized).6,8 Bowel wall was labeled as thickened if it was >3mm.6 Small bowel feces sign appeared as feces like material blended with gas in the dilated small bowel loop.8,11 Transition point is labelled when there is tapering of dilated small bowel loop to collapsed small bowel at the site of obstruction. When transition point has abrupt tapering and resembles to beak is labelled as beak sign.11,12 Patients were followed for operative findings and CT scan findings were compared with them. Final outcome was recorded on the approved Proforma.
A database was established using SPSS version 25.0 to analyze the collected data. Quantitative variables, such as age and the diameter of the dilated small bowel, were computed as mean and standard deviation. For qualitative variables, including gender, cause of obstruction, diagnosis on CT scan, and operative findings, percentages and frequencies were determined. The performance metrics, namely accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of contrast-enhanced CT abdomen in identifying SBO, were calculated with operative findings serving as the gold standard. Post-stratification 2x2 tables were generated to determine these outcomes, considering true positive (TP), true negative (TN), false positive (FP), and false negative (FN) values in this study. The level of significance was set at <0.05.
RESULTS
Two hundred and sixty-seven patients were enrolled to determine the diagnostic accuracy of CT scan in SBO taking operative findings as gold standard. There were 162 (60.7%) males and 105 (39.3%) females with overall mean age of 33.03±10.58 years (age range: 18 – 50 years). Overall 45% of patients were older than 35 years and 55% were ≤ 35 years. The mean duration of symptoms was 12.11±4.13 days among which 69% of patients presented within 14 days of onset of symptom. The mean small bowel diameter on CT scan was 3.20±0.57 cm.
Figures 1 and 2 further enhance the understanding, with figure 1 demonstrating diffuse circumferential mural thickening of the terminal ileum and ileocecal junction causing proximal small bowel dilatation, while figure 2 reveals a large midline defect in the anterior abdominal wall, leading to herniation of dilated small bowel loops and omental fat, resulting in closed-loop obstruction.
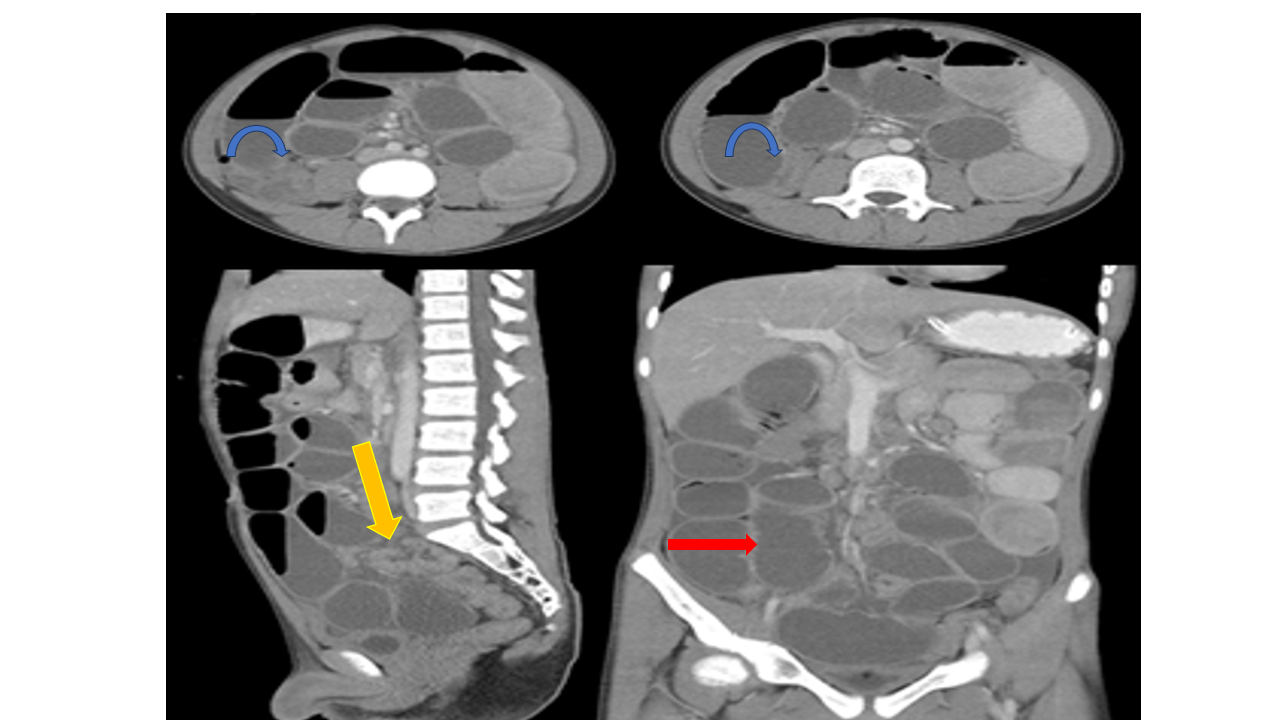
Figure 1: Multiplanar images of CECT Abdomen showing diffuse circumferential mural thickening of terminal ileum and ileocecal junction (blue arrow) causing proximal dilatation of small bowel loops (red arrow) with collapsed large bowel (yellow arrow).
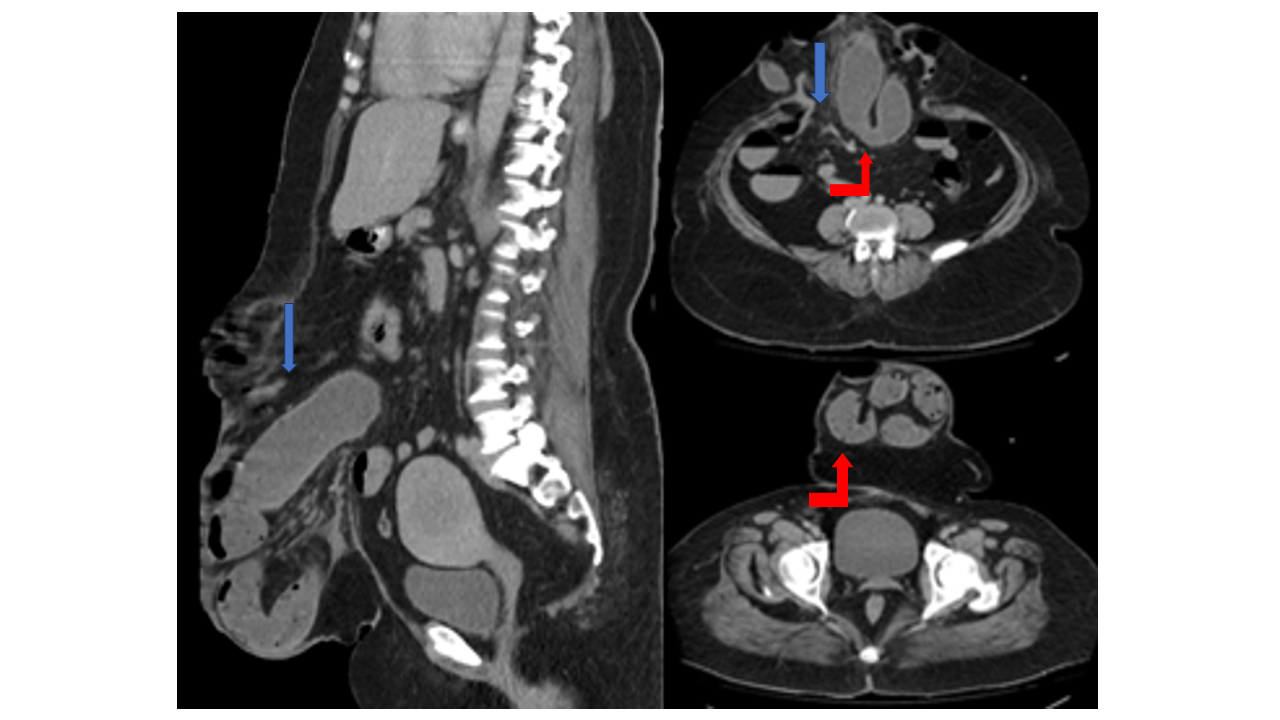
Figure 2: Sagittal and axial sections of CECT Abdomen demonstrated a large midline defect in the anterior abdominal wall (blue arrow) through which the dilated small bowel loops (red arrow) and omental fat are herniating leading to closed loop obstructio
Table 1 illustrates the common CT scan findings in small bowel obstruction, which include dilated small bowel loops (128 cases, 100%), the point of transition (105 cases, 82%), and bowel wall thickening (71 cases, 55.5%).
Table I: Distribution of CT findings in small bowel obstruction (n=128)
|
CT findings |
Frequency |
Percentage |
|
Dilated small bowl loops |
128 |
100 |
|
Point of Transition |
105 |
82 |
|
Bowl wall thickening |
71 |
55.5 |
|
Feces sign |
53 |
41.4 |
|
Beak sign |
45 |
35.2 |
|
Masses |
30 |
23.4 |
In a cohort of 267 patients, enhanced CT scans indicated SBO in 128 (47.9%) cases and ruled out SBO in 139 (52.1%) cases. Of those diagnosed with SBO on CT, 118 (92.2%) were confirmed to have the obstruction upon surgical evaluation, as noted in Table II.
Table II: Diagnostic accuracy of small bowel obstruction diagnosed on enhanced CT scan with operative findings as gold standard (n=267)
|
Enhanced CT Scan |
Operative Findings |
P Value |
||
|
Yes |
No |
Total |
<0.001** |
|
|
Yes |
118 (92.2) |
10 (7.8) |
128 |
|
|
No |
17 (12.2) |
122 (87.8) |
139 |
|
|
Total |
135 |
132 |
267 |
|
*Chi square test; **P-Value ≤0.05 considered as significant.
Sensitivity= 92.2%; Specificity=87.8%; Positive predictive value=87.4%; Negative predictive value =92.4%; Accuracy=89.88%
This highlights the notable diagnostic accuracy of enhanced CT scans, evidenced by a sensitivity of 92.2%, a specificity of 87.8%, a positive predictive value (PPV) of 87.4%, a negative predictive value (NPV) of 92.4%, and an overall diagnostic accuracy of 89.9%. Post stratification analysis according to age and gender was shown in Table III.
Table III: Diagnostic accuracy of small bowel obstruction diagnosed on enhanced CT scan with operative findings as gold standard according to age and gender (n= 267)
|
Variables |
≤ 35 years |
>35 years |
Male |
Female |
|
Sensitivity |
87.7% |
87.0% |
83.3% |
93.0% |
|
Specificity |
93.8% |
91.0% |
90.5% |
95.8% |
|
Positive predictive value |
94.6% |
88.6% |
89.0% |
96.0% |
|
Negative predictive value |
85.9% |
89.7% |
85.0% |
92.0% |
|
Diagnostic Accuracy |
90.4% |
89.2% |
87.0% |
94.3% |
Among the patients with a CT diagnosis of SBO, only 118 out of 128 had their diagnosis confirmed through surgery, while the remaining 10 did not exhibit obstruction upon operative investigation. Conversely, of the 139 patients initially deemed free of obstruction by CT, 17 were later subjected to laparotomy due to worsening clinical symptoms, revealing SBO. Within this subgroup, diagnoses included peritonitis in seven patients, enteric fever in six, and colonic carcinoma in four.
In this study, the predominant histopathological cause of SBO was tuberculosis, identified in 35 patients (25.9%). This was followed by obstructed/strangulated hernias in 30 cases (22.2%) and adhesions in 24 (17.7%) patients (Table IV).
Table IV: Primary etiologies of small bowel obstruction on histopathology
|
Primary Cause of Small Bowel Obstruction |
Frequency (n=135) |
Percentage |
|
Tuberculosis |
35 |
25.9 |
|
Hernia |
30 |
22.2 |
|
Adhesions |
24 |
17.8 |
|
Inflammation |
22 |
16.3 |
|
Small bowel malignancy |
12 |
8.9 |
|
Large bowel malignancy |
10 |
7.4 |
|
Miscellaneous (Crohn’s disease and superior mesenteric artery syndrome) |
2 |
1.5 |
DISCUSSION
This study, involving 267 patients, assessed the diagnostic accuracy of CT scans in SBO. Enhanced CT scans exhibited a sensitivity of 92.2%, specificity of 87.8%, and an overall diagnostic accuracy of 89.9%, confirming SBO in 47.9% and ruling it out in 52.1% of cases. Post-operative analysis revealed 118 out of 128 confirmed cases and 17 additional cases initially missed by CT. Tuberculosis emerged as the leading histopathological cause (25.9%), followed by obstructed/strangulated hernias (22.2%) and adhesions (17.7%). These findings highlight the clinical and diagnostic nuances in SBO management.
Bowel obstruction is a frequent surgical emergency in Pakistan as well as worldwide. It is responsible for approximately 20% of patients presented with acute abdomen in which obstruction to the small bowel remains the dominant cause with significant morbidity and mortality.1,6 Patients with clinical features of acute small bowel loop obstruction mostly undergo abdominal radiography as first line imaging modality however its diagnostic accuracy is not high with reported specificity and sensitivity of 57 % and 69% respectively.1,13 This is even lower in the diagnosis of exact site and cause of obstruction or presence of strangulation.1
Among the cross-sectional imaging modalities, CT has the potential to play a crucial role in diagnosing SBO along with its potential complications due to its multiplanar reformation and short acquisition time, which overcome bowel movement artifacts. It assesses the site and level of obstruction, which provides a road map for surgical planning. A CT scan is usually recommended when the clinical features or initial radiographic signs are equivocal or when there is suspicion of strangulation.6,12 CT scan not only diagnoses the SBO by identifying the dilated small bowel loops with/without transition point, feces sign or beak sign but also detects its various causes whether intraluminal, extraluminal or mural, like adhesions, tuberculosis, Crohn’s disease, closed loop obstruction, and hernias, among which adhesions are more prevalent culprit.11,13,14 Adhesions are generally not appreciated on CT, so they are assessed by identifying an abrupt transition from dilated to collapsed bowel without any detectable cause, giving a beak sign. The beak sign can also be appreciated in internal hernias when the bowel is trapped in mesenteric rent.8 Our study detected a beak sign in 35.1%. The point of transition, an important CT sign in SBO, was identified in 82% of cases, which is comparable to the- studies8,13,15,16 who all concluded that it can be used as a pre-surgical localizing tool for SBO. Small bowel feces sign is seen in 41.4% of our cases; literature revealed that small bowel feces sign is neither sensitive nor specific to diagnosing SBO and can be seen in patients without obstruction but when present, it is seen just proximal to transition point, which helps in its localization.8,17
This study showed overall sensitivity, specificity, PPV, NPV, and diagnostic accuracy of 87.4%, 92.4%, 92.2%, 87.8%, and 89.88%, respectively. These results were comparable with a study done by Tabassum et al.18 in terms of sensitivity of 89 % and specificity of 90.2%, with a diagnostic accuracy of 89 %. However, the NPV in this study was 87.8%, which was quite higher than theirs, which was 77%. A higher NPV is very important in excluding the presence of SBO which has marked impact on management plans. A large meta-analysis by Li Z, et al.,19 demonstrated the sensitivity and specificity of CT scan for SBO at 91% and 89%, respectively, and by Mubarak et al.6 who found a sensitivity of 95.1%, a specificity of 96.7%, a PPV of 98.7%, an NPV of 87.9%, and a diagnostic accuracy of 69.4%. The possible reason for this variation may be the difference in the level of obstruction in the two series and the difference in the relative distribution of adhesions and hernia as underlying causes.
The current study missed four cases of colonic carcinoma causing partial/intermittent obstruction. Mubarak SA, et al.,6 also missed the colonic carcinoma at splenic flexure in a patient in their study of 111 patients. Vaughan-Shaw PN, et al.,20 also concluded that a CT scan can miss or incorrectly diagnose colorectal carcinoma when the tumor is small in size or the CT is done with poor bowel preparation. Lack of peritumoral findings like fat stranding, vessel engorgement, and enlarged lymph nodes can also contribute to miss the lesion.20,21
The etiology of mechanical bowel obstruction is changing in our population, which may be due to different eating habits and the influence of genetic as well as environmental factors. The study done by Elsayed EE, et al.,22 on a small group of 20 Egyptian patients showed adhesions and obstructed hernia as the leading causes of SBO, comprising 37% and 27% of cases, respectively. A local study reported adhesions (57.8%) as the main cause of SBO, followed by hernia (16.7%) and tuberculosis (15.7%).9 Mubarak SA, et al., 6 showed tuberculous stricture in the majority of cases (35.8%), followed by adhesions (26.0%) and hernia (18.5%). The present results are comparable in terms of cause of SBO with the study done by Mubarak SA, et al., 6, as in this study group, the most common cause identified is tuberculosis (25.9%), followed by hernia (22.2%) and adhesions (17.7%), representing the burden of tuberculous infection in the local population and delay in management of hernia. Other causes of SBO in this study were post pancreatitis, post appendicitis, ileitis, peritonitis, small bowel malignancy, cecal carcinoma, proximal large bowel carcinoma, Crohn’s disease, and SMA syndrome. However, CT scans missed the diagnosis of peritonitis in three cases, colonic carcinoma in two cases, and typhoid fever in two cases. So these fallacies must be kept in mind, and the clinical context should not be ignored.
Most previous studies have shown variable sensitivity, specificity, and accuracy,6,18,19 which were comparable to the current study, which showed a sensitivity of 92.2%, a specificity of 87.8%, and an accuracy of 89.88%. These results are quite satisfactory in diagnosing the SBO in the local practice setup where health care resources are limited. This study also helped in the timely management of patients by avoiding unnecessary surgical interventions. A CT scan should be included in workup of acute abdomen, particularly when SBO is suspected.
This study has as few limitations, including its single-center design and cases where conservative management introduced uncertainty in the diagnosis. Nevertheless, it contributes valuable local evidence regarding the judicious use of imaging in abdominal conditions. Future research should consider a multi-center approach, focusing on the nuanced role of CT findings in SBO, both within and beyond the bowel.
CONCLUSION
CT scan emerges as a promising imaging tool for the accurate detection of SBO, offering heightened accuracy, sensitivity, and specificity. It proves valuable in delineating the level and cause of acute SBO, aiding in the identification of patients managed conservatively and preventing unnecessary surgeries. Therefore, CT scans should be considered the primary imaging modality for suspected SBO. However, it is crucial to exercise clinical judgment, particularly in cases of peritonitis and typhoid fever, where clinical findings play a pivotal role.
REFERENCES
1. Sultan A, Hassan M, Ali M. Role of multidetector computed tomography with multiplanar and curved multiplanar reformations in the detection of cause of intestinal obstruction: a tertiary care experience. Cureus 2020;12(3):e7464. https://doi.org/10.7759/cureus.7464
2. Afzal S, Ahmad F, Farooq F. Role of multi-detector computed tomography in the diagnosis of intestinal obstruction. Cureus 2023;15(1):e33730. https://doi.org/10.7759/cureus.33730
3. Ojo EO, Ihezue CH, Sule AZ, Ismaila OB, Dauda AM, Adejumo AA. Aetiology, clinical pattern and outcome of adult intestinal obstruction in JOS, north central Nigeria. Afr J Med Med Sci 2014;43(Suppl 1):29-33.
4. Mullan CP, Siewert B, Eisenberg RL. Small bowel obstruction. AJR Am J Roentgenol 2012;198(2):W105-17. https://doi.org/10.2214/ajr.10.4998
5. Aregawi AB, Alem AT, Girma A. A rare case of intestinal tuberculosis with chronic partial small bowel obstruction in a 37-year-old ethiopian man. Int Med Case Rep J 2022;15:725-33. https://doi.org/10.2147/imcrj.s388269
6. Nayab S, Ali SM, Jesrani A, Raza ML, Zaidi SMH. Diagnostic accuracy of CT scan in detecting intestinal obstruction keeping the histopathology findings as gold standard. Ann Abbasi Shaheed Hosp Karachi Med Dent Coll 2016;21(1):17-22.
7. Soressa U, Mamo A, Hiko D, Fentahun N. Prevalence, causes and management outcome of intestinal obstruction in Adama Hospital, Ethiopia. BMC Surg 2016;16(1):38. https://doi.org/10.1186/s12893-016-0150-5
8. Paulson EK, Thompson WM. Review of small-bowel obstruction: the diagnosis and when to worry. Radiology 2015;275(2):332-42. https://doi.org/10.1148/radiol.15131519
9. Memon W, Khattak YJ, Alam T, Sconfienza LM, Awais M, Anwar SSM. MDCT of small bowel obstruction: How reliable are oblique reformatted images in localizing point of transition? Gastroenterol Res Pract 2014;2014:1-7. https://doi.org/10.1155/2014/815802
10. Mallo RD, Salem L, Lalani T, Flum DR. Computed tomography diagnosis of ischemia and complete obstruction in small bowel obstruction: a systematic review. J Gastrointest Surg 2005;9(5):690-4. https://doi.org/10.1016/j.gassur.2004.10.006
11. Nicolaou S, Kai B, Ho S, Su J, Ahamed K. Imaging of acute small-bowel obstruction. ARJ Am J Roentgenol 2005;185(4):1036-44. https://doi.org/10.2214/ajr.04.0815
12. Mohi JK, Kajal S, Singh T, Singh J, Kaur N. Role of imaging in evaluation of intestinal obstruction. Int J Med Res Rev 2017;5(6):593-603.
13. Iqbal A, Shahzad S, Gul P, Kumar B. To determine the diagnostic accuracy of curved multiplanar reformat of multidetector CT scan in visualizing zone of transition in patients with intestinal obstruction. J Liaquat Uni Med Health Sci 2017;16(1):37-40. https://doi.org/10.22442/jlumhs.171610503
14. Hassan M, Ali M, Shazlee MK, Bughio S, Raza F, Haroon F. Detection of transition zone in bowel obstruction via curved multiplanar reformations with multidetector computed tomography. Cureus 2019;11(3):e4233. https://doi.org/10.7759/cureus.4233
15. Shaikh M, Sahito AA, Azeem N, Khan A, Shaikh AH, Memon SA. Diagnostic accuracy of CT scan in detection of point of transition of small bowel obstruction. Ann Punjab Med Coll 2022;16 (1):33-6. https://doi.org/10.29054/apmc/2022.1037
16. Idris M, Kashif N, Idris S, Memon WA, Tanveer UH, Haider Z. Accuracy of 64-slice multidetector computed tomography scan in detecting of the point of transition of small bowel obstruction. Jpn J Radiol 2012;30(3):235-41. https://doi.org/10.1007/s11604-011-0038-3
17. Lazarus DE, Slywotsky C, Bennett GL, Megibow AJ, Macari M. Frequency and relevance of the "small-bowel feces" sign on CT in patients with small-bowel obstruction. AJR Am J Roentgenol 2004;183(5):1361-6. https://doi.org/10.2214/ajr.183.5.1831361
18. Khatib S, Tabassum S, Urooj T, Haider S, Mehmood T. Diagnostic accuracy of multi-detector ct scan in detection of ‘point of transition’ in small bowel obstruction. Pak J Radiol 2019;29(2):108-12.
19. Li Z, Zhang L, Liu X, Yuan F, Song B. Diagnostic utility of CT for small bowel obstruction: Systematic review and meta-analysis. PLoS One 2019;14(12): e0226740. https://doi.org/10.1371/journal.pone.0226740
20.Vaughan-Shaw PG, Aung M, Knight H, Williams T, Borley NR, Wheeler JMD. Systematic analysis of missed colorectal cancer cases and common pitfalls in diagnosis. Frontline Gastroenterol 2015;6(4):232-40. https://doi.org/10.1136/flgastro-2014-100513
21. Klang E, Eifer M, Kopylov U, Belsky V, Raskin S, Konen E, et al. Pitfalls in diagnosing colon cancer on abdominal CT. Clin Radiol 2017;72(10):858-63. https://doi.org/10.1016/j.crad.2017.06.007
22. Elsayed EE, Habib RM, Soltan BS. Role of multidetector computed tomography in the diagnosis of intestinal obstruction. Menoufia Med J 2018;31:1465-2. https://doi.org/10.4103/mmj.mmj_194_16.
|
CONFLICT OF INTEREST Authors declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work.
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |