![]() https://doi.org/10.35845/kmuj.2023.23046 ORIGINAL
ARTICLE
https://doi.org/10.35845/kmuj.2023.23046 ORIGINAL
ARTICLE
ASSESSMENT OF RADIOLOGICAL HEALING IN ELDERLY HIP FRACTURES FIXED WITH INTRAMEDULLARY VERSUS EXTRAMEDULLARY IMPLANTS AT THREE MONTHS
Israr ul Haq 1, Muhammad Bilal 1, Noman Ali 1, Inayat ur Rehman 1,
Syed
Imran Bukhari 1![]()
|
1: Department of Trauma & Orthopedics, Medical Teaching Institution Lady Reading Hospital, Peshawar, Pakistan.
Email
Contact #: +92-333-9630619 Date Submitted: August14, 2022 Date Revised: March12, 2023 Date Accepted: March 15, 2023 |
|
THIS ARTICLE MAY BE CITED AS:Haq IU, Bilal M, Ali N, Rehman IU, Bukhari SI.Assessment of radiological healing in elderly hip fractures fixed with intramedullary versus extramedullary implants at three months. Khyber Med Univ J 2023;15(1):26-30. https://doi.org/10.35845/kmuj.2023.23046 |
ABSTRACT
OBJECTIVE: To compare the radiological healing in elderly patients with hip fractures fixed with intramedullary versus extramedullary implants at 3 months by using Radiological Union Score for Hip (RUSH score).
METHODS: This quasi-experimental study was conducted at Lady Reading Hospital, Peshawar from September 2020 to March 2021, in elderly patients (50-80 years) with hip fractures. Out of 238 patients, 119 were non-randomly assigned to Group-A undergoing intra- medullary implants and 119 to Group-B undergoing fixation with an extra-medullary implant. After the surgery, the patients were followed up periodically at 2nd week, 6th week and 12th week after surgery and assessed for radiological healing through RUSH score. The data was analyzed using SPSS version 23.
RESULTS: Out of 238 patients, 96 were males and 142 were females. In Group-A, 51 (42.9%) were males and 68 (57.1%) were females. In Group-B, 45 (37.8%) were males and 74 (62.2%) were females. Majority (n=135/238: 56.72%) were aging from 50-60 years. Mean±SD of age was 63.1±8.8 years and 61.7±8.1 years in Group-A & Group-B respectively. Mean±SD of RUSH score in Group-A & Group-B was 19.50±6.92 and 22.51±5.60 respectively.Mean RUSH score for males in Group-A and Group-B was 21.52±6.39 and 22.33±6.99 (p=0.354) and for females in Group-A and Group-B was 19.36±7.33 and 22.18±5.75 (p=0.025) respectively.Median and IQR of RUSH score in Group-A & Group-B was 21±10 and 23±8 respectively (p=0.069).
CONCLUSION: There was statistically insignificant difference in median RUSH score with use of either intramedullary or extramedullary implants in the management of hip fractures.
Clinical Trial Registration Number: ACTRN12623000103662
KEYWORDS: RUSH score (Non-MeSH); Hip Joint (MeSH); Hip Fractures (MeSH); Intramedullary (Non-MeSH); Extramedullary (Non-MeSH);Geriatric hip fractures (Non-MeSH);FemoralFracture (MeSH); Femoral Neck Fractures (MeSH).
INTRODUCTION
Patients sustaining proximal femur fractures pose a major challenge to the health care team due to the old age group that majority of such patients belong to, related risk factors, prolonged period of recovery and high mortality rate.1,2Ninety-five percent of proximal femur fractures in elderly patients are due to fall.3 There is a high risk of mortality after proximal femur fractures particularly in elderly patients 60 years of age or above. According to one study, overall 1-year mortality in patients ≥60 years of age treated after proximal femur fractures was 21%. In another research overall 1-year postoperative mortality was 27%.4,5
Various scores have been introduced to assess radiological healing of hip fractures after surgery. One of these scores is the Radiological Union Score for Hip (RUSH score). This score uses a checklist-based approach. It improves agreement of fracture healing assessment among healthcare personnel, offers a systematic approach to evaluate hip fracture radiographs and provides prognostic information that can predict healing outcomes.6 It is a validated outcome instrument designed to improve intra and inter-observer reliability in describing healing of hip fracture.7
Depending on the fracture type and clinicians’ preference, different surgical procedures are chosen to manage these fractures, in order to achieve the best outcomes considering the fracture and patient characteristics. The commonest procedures use intramedullary and extra medullary implants for the management of hip fractures.8 There is lack of evidence regarding comparison of these procedures in terms of radiological healing outcome using validated outcome assessment tool. FAITH trial investigators reported that for every 1 unit decrease in RUSH, there was a 2% increase in odds of reoperation within 24 months of the fracture; for every 2 units decrease in RUSH, 5% increase in risk of reoperation and for every 5 units decrease in RUSH, 14% increase in odds of reoperation.9
Recently a cohort study conducted by Ahmed T, et al showed that there was no significant difference in terms of radiological healing between intramedullary and extramedullary implants group at 6 months on the basis of RUSH score, however the number of patients in the intramedullary group was very small.10
The rationale of this study was to address the question (knowledge gap) which is still unanswered in that how radiological healing, assessed via RUSH score (validated outcome assessment instrument), will be affected by intramedullary or extramedullary implants at 3 months in patients with hip fracture. We plannedthis quasi-experimentalstudy to assess which method of surgical fixation (intramedullary or extramedullary) gives better outcomes at 3 months using RUSH score. The results of this study will help orthopaedic surgeons in deciding which of these two methods is better suited for management of elderly patients with hip fracture.
METHODS
This Quasi-experimental study was conducted at Orthopedics department of Lady Reading Hospital, Peshawar, Pakistan. Our hypothesis was thatthere is a difference in radiological healing of hip fracture at 3 months fixed with either intramedullary or extramedullary implants. Previous literature on RUSH score has used mean values for assessment. For sample size calculation, we used mean values but we will report median values as well as RUSH is an ordinal scale.We assumed that at 3 months, mean RUSH score will be 22±5.5 for extramedullary implants and 20±5.5 for intramedullary implants.10 With probability of type 1 error at 0.05, type 2 error at 0.2, power of 0.8, our calculated sample size was 238 (119 in each group).
Inclusion criteria was patients of both genders with age group 50-80 years, having hip fracture (Transcervical, Intertrochanteric and Subtrochanteric) as per standard definitions. Patients with following characteristics were excluded; refusal of informed consent,unwilling/unable to comply with follow up, polytrauma, history of steroids use, history of use of immunosuppressants/disease modifying anti-rheumatic drugs (DMARDs), pathological fracture and unfit for surgery (ASA III and above).
The study was conducted after getting approval from hospital ethical and research committee. Study duration was six months (September 2020 to March 2021). The patients meeting the inclusion criteria in the orthopaedics ward of Lady Reading Hospital, Peshawar were recruited in the study after taking written informed consent. The diagnosis of hip fracture was made based upon the criteria mentioned in the inclusion criteria. Sampling technique was non-probability, consecutive sampling. The purpose of the study and what this study entails were explained to all the recruited patients at the start of the study before enrolling them. Demographic data including age and gender of the patient was noted. History was taken from the patient to find out the duration of the injury. Routine baseline investigations were performed and these patients were prepared for surgery.
The surgery involved extramedullary (dynamic hip screw, dynamic condylar screw, cannulated screws, proximal femoral locking plate) implants in half of the patients and fixation with an intramedullary (proximal femoral nail, gamma nail) implant in the other half via non-randomized protocol (Figure 1 &2).
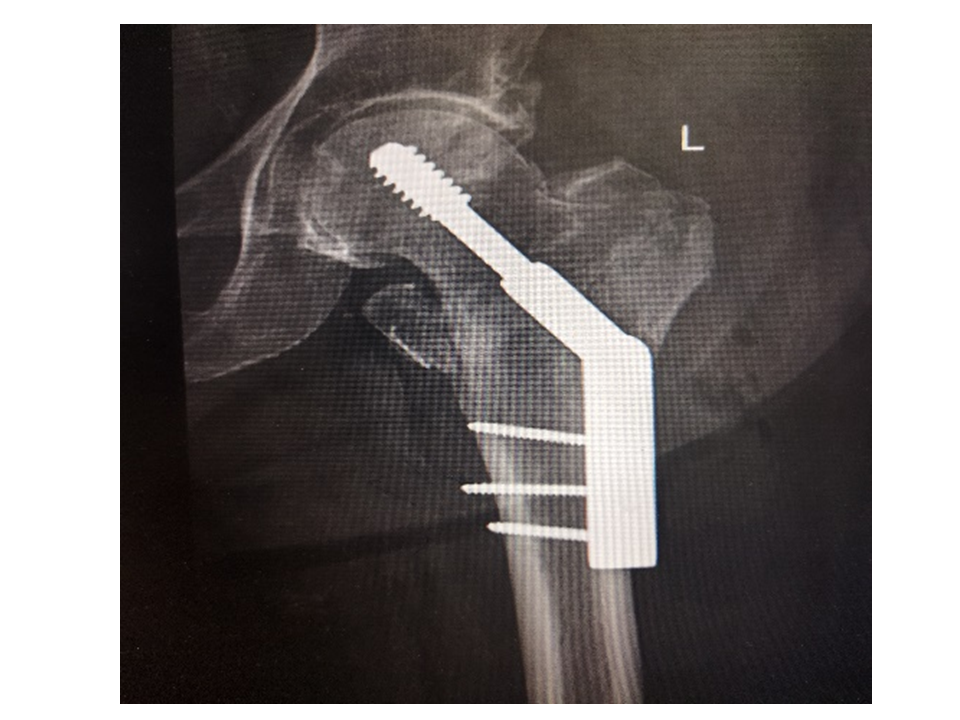
Figure 1: Extramedullary implant

Figure 2: Intramedullary implant
After the surgery, the patients were followed up periodically at 2nd week, 6th week and 12th week after surgery to look for radiological healing. X-rays of the hip were performed at the time of follow up and RUSH score was used to assess for radiological healing. All the data was recorded on a predesigned proforma for analysis. Figure 3: Methodology flow diagram of the study is given in Figure 3.
Figure
3: Methodology flow diagram of the study The data was analyzed using SPSS version 23. Frequencies and percentages were used to describe
categorical variables such as gender. Mean and standard deviation were
calculated for the numerical variables for age. Mann- Whitney test was used to
compare the means of RUSH scores in two groups and a p-value of less than 0.05 was
taken as significant. Median and IQR was calculated for both groups and Wilcoxon
rank sum test was used compare the medians with p value of < 0.05 as
significant. The trial has been registered with anzctr.org.au (Trial
ID-ACTRN12623000103662). RESULTS A
total of 238 patients with 96 (40.36%) males and 142 females (59.64%) were
included in the study.Each group (Group A: intramedullary implant and Group B: extramedullary
implant) included 119 patients to compare the radiological healing in elderly
patients with hip fractures at 3 months using RUSH score. Mean±SD of age in
intramedullary implants group was 63.1±8.7 with 95% C.I (61.5-64.7) and
extramedullary implants group was 61.7±8.1 with CI (60.23-63.18) years.Mean±SD
of RUSH score in intramedullary (Group-A) and extramedullary implants (Group-B)
was 19.50±6.92(CI,18.25-20.76) and 22.51±5.6 (CI,21.49-23.53), respectively (Table
I). Variables Minimum Maximum Mean S.D 95%
CI Age (years) Group A (Intramedullary
Implants) (n=119) 50 80 63.1 8.8 61.50-64.69 Group B (Extramedullary
Implants) (n=119) 50 80 61.7 8.1 60.22-63.17 RUSH Score Group A (Intramedullary
Implants) (n=119) 3 30 20.3 7.0 19.02-21.57 Group B (Extramedullary
Implants) (n=119) 3 30 22.2 6.2 21.07-23.32 Mean
RUSH score for males in Group-A and Group-B was 21.52±6.39 and 22.33±6.99
(p=0.354) and for females in Group-A and Group-B was 19.36±7.33 and 22.18±5.75
(p=0.025) respectively. Stratification of age group, gender and duration of
fracture with rush score between groups is presented in Table II. Median and
IQR of RUSH score in intramedullary(Group A) and extramedullary implants (Group-B)
was 21±10 and 23±8 (p value <0.069). TABLE II: STRATIFICATION
OF AGE GROUP, GENDER AND DURATION OF FRACTURE WITH RUSH SCORE BETWEEN GROUPS Variables RUSH
SCORE P-VALUE Mean SD Mean Rank Mann
Whitney U Age
Group (years) 50 - 60 Intramedullary Implants (n=65) 19.80 7.34 60.36 1778.500 0.028 Extramedullary Implants (n=70) 22.34 6.66 75.09 >60 Intramedullary Implants (n=54) 20.89 6.58 50.03 1216.500 0.480 Extramedullary Implants (n=49) 22.10 5.60 54.17 Gender Male (n=96) Intramedullary Implants (n=51) 21.52 6.39 46.03 1021.500 0.354 Extramedullary Implants (n=45) 22.33 6.99 51.30 Female (n=142) Intramedullary Implants (n=68) 19.36 7.33 63.47 1970.000 0.025 Extramedullary Implants (n=74) 22.18 5.75 78.88 Duration (days) 2 -12 Intramedullary Implants (n=55) 19.92 7.55 55.06 1488.500 0.187 Extramedullary Implants (n=63) 21.79 6.57 63.37 >12 Intramedullary Implants (n=64) 20.60 6.53 55.12 1447.500 0.069 Extramedullary Implants (n=56) 22.75 5.83 66.65 Applied Mann Whitney test DISCUSSION This
study shows that the median RUSH score was not significantly different at 3
months in intramedullary group compared to the extramedullary group with p
value of 0.069. An estimated fifty
million musculoskeletal injuries occur annually in the United States with six
million of those being fractures.11 Approximately 10% of those
fractures result in non-union.12 Clinicians & researchers have
often failed to agree on relevant and reproducible measures of fracture
healing.11 Although most surgeons believe fracture healing should be
determined using clinical and radiographic information, there is significant variability
in the methods for assessing fracture healing in practice.12Given
the myriad criteria and lack of consensus, generalizability of results is
lacking. The assessment of femoral neck fracture healing remains highly
subjective and causes disagreements among treating physicians.13 The decision of whether
to use intramedullary or extramedullary implants for the management of hip
fractures is dependent on multiple factors, including bone quality, fracture
pattern, surgeon expertise and available resources. There is a general trend towards
intramedullary fixation of late, but the question whether intramedullary
implants work as well as extramedullary implants is unanswered, using validated
criteria. The Radiographic Union
Score for Hip (RUSH) is a validated tool that improves fracture healing
agreement between radiologists and orthopaedic surgeons by using a
checklist-based scoring approachwith improved intra- and interobserver
reliability.14,15 The utilization of this tool to assess femoral
neck fracture healing has led to better agreement with respect to radiographic
healing as well as improved interobserver and intraobserver reliability .6
Two reviewers in previous study assessed 250 hip fractures 6 months post operatively
by assigning RUSH scores and demonstrated substantial interobserver reliability
with an ICC of 0.81 . Their study also found that a threshold of RUSH < 18
was associated with 100% specificity and a positive predictive value of 100%
for radiographic nonunion.7 In this study, mean age
in intramedullary implants group was 63.1±8.8 and in extramedullary implants
group was 61.7±8.1 years. The study of Frank T, et al reported mean age to be
71±12.7 This is generally in line with average life expectancy in
this region notwithstanding ten years difference in the mean age group. In their study, Frank T,
et al noted RUSH score as 22.9±4.2 versus 24.8±3.0, with a significant p-value
of 0.002.7Present study noted mean radiological union scale for hip
(RUSH) score as 19.50±6.9 and 22.51±5.60 in intramedullary and extramedullary
implants group with significant p-value, 0.029. The determination of bony union
is essential for clinical care as well as research purposes to evaluate various
treatment methods. Our study uses validated fracture assessment method. Traditionally,
extramedullary implants have given good results. Shifting to use of intramedullary
techniques to address these fractures entails training and expertise and good
instrumentation. In absolute terms, RUSH is an ordinal scale and it is just
reasonable to report median values for the groups, and the difference is
insignificant (0.069) in this study. The strength of this study is that we have
reported both mean and median values for the groups. Limitations of this study
are inherent in the study design. We could not go for randomized controlled
trial (RCT) because of equipoise with use of intramedullary implants in the
management of hip fractures. In future, well designed RCT will help address our
limitation. CONCLUSION There
was statistically insignificant difference in median RUSH score with use of
either intramedullary or extramedullary implants in the management of hip
fractures. ACKNOWLEDGMENTS All the patients who consented
to be enrolled in this study. REFERENCES 1.
Haleem
S, Lutchman L, Mayahi R, Grice JE, Parker MJ. Mortality following hip fracture:
trends and geographical variations over the last 40 years. Injury2008;39(10):1157-63.https://doi.org/10.1016/j.injury.2008.03.022 2. Haentjens P,
Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al.
Meta-analysis: excess mortality after hip fracture among older women and men.
Ann Intern Med2010;152(6):380-90.https://doi.org/10.7326/0003-4819-152-6-201003160-00008 3.
Nyberg
L, Gustafson Y, Berggren D, Brännström B, Bucht G. Falls leading to femoral
neck fractures in lucid older people. J Am Geriatr Soc1996;44(2):156-60.https://doi.org/10.1111/j.1532-5415.1996.tb02432.x 4.
Panula
J, Pihlajamäki H, Mattila VM, Jaatinen P, Vahlberg T, Aarnio P, Kivelä SL.
Mortality and cause of death in hip fracture patients aged 65 or older-a
population-based study. BMC Musculoskelet Disord2011;12(1):1-6.https://doi.org/10.1186/1471-2474-12-105 5.
Schnell
S, Friedman SM, Mendelson DA, Bingham KW, Kates SL. The 1-year mortality of
patients treated in a hip fracture program for elders. Geriatr Orthop Surg
Rehabil 2010;1(1):6-14.https://doi.org/10.1177/2151458510378105 6. Chiavaras MM,
Bains S, Choudur H, Parasu N, Jacobson J, Ayeni O, et al. The Radiographic
Union Score for Hip (RUSH): the use of a checklist to evaluate hip fracture
healing improves agreement between radiologists and orthopedic surgeons. Skelet
Radiol2013;42(8):1079-88.https://doi.org/10.1007/s00256-013-1605-8 7. Frank T, Osterhoff
G, Sprague S, Garibaldi A, Bhandari M, Slobogean GP. The Radiographic Union
Score for Hip (RUSH) identifies radiographic nonunion of femoral neck fracture.
Clin Orthop Relat Res2016;474:1396-404.https://doi.org/10.1007/s11999-015-4680-4
8. Butler M, Forte
ML, Joglekar SB, Swiontkowski MF, Kane RL. Evidence summary: systematic review
of surgical treatments for geriatric hip fractures. J Bone Joint Surg Am
2011;93(12):1104-15.https://doi.org/10.2106/JBJS.J.00296 9. Bernaus M,
Slobogean GP, Bzovsky S, Heels-Ansdell D, Zhou Q, Bhandari M, et al. Early
Radiographic union score for hip is predictive of femoral neck fracture
complications within 2 years. J Orthop Trauma2020;34:195-202.https://doi.org/10.1097/BOT.0000000000001713 10.
Ahmad
T, Muhammad ZA, Habib A. Injury specific trauma registry: outcomes of a
prospective cohort with proximal femur fractures. Ann Med Surg 2019;1;45:54-8.https://doi.org/10.1016/j.amsu.2019.07.015 11.
Einhorn TA. Enhancement of fracture-healing. J
Bone Joint Surg Am 1995 Jun;77(6):940-56. https://doi.org/06/00004623-199506000-00016 12. Meling T, Harboe K, Søreide K. Incidence of traumatic long-bone
fractures requiring in- hospital management: a prospective age- and gender-specific
analysis of 4890 fractures. Injury 2009 Nov;40(11):1212-9. https://doi.org/10.1016/j.injury.2009.06.003 12. FAITH Investigators.
Fixation using alternative implants for the treatment of hip fractures (FAITH):
design and rationale for a multi-centre randomized trial comparing sliding hip
screws and cancellous screws on revision surgery rates and quality of life in
the treatment of femoral neck fractures. BMC Musculoskelet Disord2014;15:219.https://doi.org/10.1186/1471-2474-15-219 13. Blomfeldt R,
Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Comparison of internal
fixation with total hip replacement for displaced femoral neck fractures.
Randomized, controlled trial performed at four years. J Bone Joint Surg
Am2005;87:1680–8.https://doi.org/10.2106/JBJS.D.02655
14.
Gullberg
B, Johnell O, Kanis JA. World-wide projections for hip fracture. Osteoporos Int
1997;7:407–13.https://doi.org/10.1007/pl00004148. 15. LiporaceFA,EgolKA,TejwaniN,ZuckermanJD,KovalKJ.What’snewinhipfractures? Current
concepts. Am J Orthop (Belle Mead NJ) 2005;34:66–74. 16. Corrales LA,
Morshed S, Bhandari M, Miclau T 3rd. Variability in the assessment of
fracture-healing in orthopaedic trauma studies. J Bone Joint Surg
Am2008;90:1862–8.https://doi.org/10.2106/JBJS.G.01580 17. Veronese N, Maggi
S. Epidemiology and social costs of hip fracture. Injury 2018;49(8): 1458–60.https://doi.org/10.1016/j.injury.2018.04.015 18. Brauer CA,
Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip
fractures in the United States. JAMA2009;302(14):1573–9.https://doi.org/10.1001/jama.2009.1462 19. Kannus P, Parkkari
J, Sievanen H, Heinonen A, Vuori I, Jarvinen M. Epidemiology of hip fractures.
Bone 1996;18(1suppl):57S–63. https://doi.org/10.1016/8756-3282(95)00381-9 20. Lewiecki EM,
Wright NC, Curtis JR, Siris E, Gagel RF, Saag KG, et al. Hip fracture trends in
the United States, 2002 to 2015. Osteoporos Int2018;29(3):717–22.https://doi.org/10.1007/s00198-017-4345-0 21. Burge R,
Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and
economic burden of osteoporosis-related fractures in the United States,
2005–2025. J Bone Miner Res2007;22(3):465–75.https://doi.org/10.1359/jbmr.061113 Following authors have made substantial contributions to the
manuscript as under: IuH, MB, NA: Acquisition
of data, drafting the manuscript, approval of the final version to be
published. IuR: Analysis
and interpretation of data, drafting the manuscript, approval of the final
version to be published. SIB: Concept
and study design, drafting the manuscript, critical review, approval of the
final version to be published Authors agree to be accountable for all aspects of the work in
ensuring that questions related to the accuracy or integrity of any part of
the work are appropriately investigated and resolved. CONFLICT
OF INTEREST Authors declared
no conflict of interest GRANT
SUPPORT AND FINANCIAL DISCLOSURE Authors declared
no specific grant for this research from any funding agency in the public,
commercial or non-profit sectors DATA
SHARING STATEMENT The data that support the findings of this study are
available from the corresponding author upon reasonable request KMUJ web
address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk
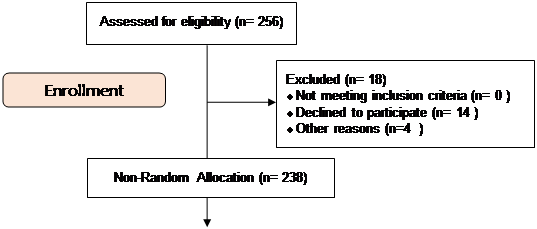
TABLE I: DESCRIPTIVE STATISTICS OF THE STUDY SUBJECTS
![]() This is an Open Access article
distributed under the terms of the Creative Commons
Attribution-Non-Commercial 2.0 Generic License.
This is an Open Access article
distributed under the terms of the Creative Commons
Attribution-Non-Commercial 2.0 Generic License.