![]() https://doi.org/10.35845/kmuj.2023.23034 STUDYPROTOCOL
https://doi.org/10.35845/kmuj.2023.23034 STUDYPROTOCOL
Effects of proprioceptive neuromuscular facilitation in addition to routine physical therapy on pain range of motion and postural alignment in patients with temporomandibular joint disorders: a randomized controlled trial protocol
Sarwat
Anees 1,2, Fareeha Amjad 3 ![]()
|
1: Punjab Social Security Health Management Company Hospital, Raiwind, Lahore, Pakistan 2: University Institute of Physical Therapy, University of Lahore, Lahore, Pakistan 3: Faculty of Rehabilitation and Allied Health Sciences, Riphah International University, Lahore, Pakistan Email Cell #: +92-334-3372779
|
|
THIS ARTICLE MAY BE CITED AS: Anees S, Amjad F. Effects of proprioceptive neuromuscular facilitation in addition to routine physical therapy on pain, range of motion and postural alignment in patients with temporomandibular joint disorders: a randomized controlled trial protocol. Khyber Med Univ J 2023;15(3):198-202. https://doi.org/10.35845/kmuj.2023.23034 |
ABSTRACT
OBJECTIVE: To evaluate the effects of proprioceptive neuromuscular facilitation (PNF) on pain, range of motion (ROM), and postural alignment in temporomandibulder joint disorders (TMD) patients with forward head posture (FHP).
METHODS: This single blinded, randomized control trial will be conducted at Physiotherapy Department, Punjab Social Security Health Management Company Hospital, Raiwind, Lahore, Pakistan. Study design will be parallel having 58 Sample size, allocation ratio 1:1. Group A (control) will follow routine physiotherapy (ultrasound/TENS and stretching/strengthening and ROM exercises for jaw and group B (intervention) will follow proprioceptive neuromuscular facilitation (PNF) program with routine physiotherapy. Both groups will follow 3 sessions per week for 4 weeks and home exercises for 2 weeks. Pain, ROM and Postural assessment will be conducted on baseline, 6th and 12th week. The PNF program will compose of a total of 8 therapeutic exercises.This exercise program will help clinician in future to treat TMD patient more effectively. Main outcome variables will be Pain , ROM and Postural assessment. Pain and ROM are primary outcome and postural assessment is secoundary outcome.pain intensity will be measured by visual analogue scale, ROM by vernier caliper and photogrammatory method will be used for postural assessment.
DISCUSSION: This randomized controlled trial will be the first of its kind for TMD due to forward head posture. this trial will provide a well structured and well planned exercise plan.
Clinical Trial Registration Number: IRCT20210704051785N1
KEYWORDS: Pain (MeSH); Range of Motion, Articular (MeSH); Postural Assessment (Non-MeSH); Pain Measurement (MeSH); Visual Analog Pain Scale (MeSH); Muscle Stretching Exercises (MeSH); Forward head posture (Non-MeSH); Temporomandibular Joint Disorders (MeSH).
INTRODUCTION
Temporomandibular disorder (TMD) causes pain around the temporomandibular joint and dysfunction of surrounding muscles. The causes of TMD can be attributed to many factors. These mainly include the pathological status of the muscles that are frequently used in chewing, the posture muscles of the neck, and the connection status of the Temporomandibular joints(TMJ).1
The causes of TMD reported in the literature varied widely, including improper chewing or other bad habits, trauma, improper postures, spinal deformation, or mental stress.2 TMD may be cause not only by the structural defects around the temporomandibular joint but also abnormal alignment of the neck or deformation, resulting in anomaly in the temporomandibular joint. Janda suggested that the structural damages in the surrounding tissues caused during the inflammatory phase after an injury is inflicted on the musculoskeletal system.3,4
TMD affects up to 15% of adults and 7% of adolescents. Incidence reports TMD pain in adult diagnosis were 3.9% and for self-reported TMD-pain in adolescents were 4.6%.5 Women suffer from TMD than men. Although there are arguably multiple reasons for sex‐related differences in the prevalence of TMD, one candidate for the increased occurrence of this disorder in women has been suggested to be the female sex hormone estrogen.6
The symptoms of TMD include excessive tension in the muscles in the chin, face, and neck, remitted movement of the chin, pain when opening or closing the mouth, and noise from the Temporomandibular joint. Due to the damages in the body structure and body functional compromises, the patients experience difficulties in swallowing, eating, chewing in daily living life.7 Cortese et al. argued that the forward headed posture changes the position of the mandible, so that the mandible is pulled posteriorly and inferiorly, while the locations of the mandibular condyle and articular disc positions are changed in temporomandibular joint.8
The forward headed posture, which was the hypothesis of the TMD of the patient, causes excessive tension in certain muscles in the head and neck, impairing the chewing and eating activities. Such an abnormal movement causes inflammation in the temporomandibular joint, making noises and causing pain.9
Analgesic drugs are primary treatment for TMD‐related pain and dysfunction with more that 90% of treatment recommendations involving use of medications. however, evidence in support of the effectiveness of these drugs is lacking.6 Extensive reviews and clinical studies do not indicate that orthodontic treatment predisposes or decreases the risk of developing future TMD. Recent studies highlight that occlusion-changing procedures are no longer considered appropriate for most patients with TMD.10
In a national survey, 72% individual considered physiotherapy as an effective treatment for TMD, jaw exercises (79%), ultrasound (52%), manual therapy (48%), acupuncture (41%) and laser therapy (15%) considered to be effective.11 De Freitas et al. (2013) reported that the home programs for TMD were effective in addressing the problems of the patients who were closely related to improper habits.12 Yagi et al. (2008) focused on the tongue movement of the TMD patients and reported that frequent hanging out the tongue may cause impairment of the temporomandibular joint. And, with the pulling of the tongue, they tried to realign the cervical spine and relax the muscles surrounding the temporomandibular joint.13
PNF was developed by Kabat and Knott, 1953 during the 1950s .14 The philosophy of PNF is to use the total body approach and the positive approach to focus on improving the activity level and the body structures and body functions.15,16 PNF is indirect treatment is effective in functional enhancement for the patients with musculoskeletal diseases accompanying severe pain.17 PNF is effective in TMD.18
Due to increased use of technology like cell phone and computers, forward head posture is a problem of modern world. According to evidence abnormal neck alignment is a cause of TMD. Patient suffering from TMD due to abnormal neck alignment from years but not having proper structural exercise plan is a major literature gap. Evidence show abnormal neck alignment or forward head posture with TMD, was effectively managed in a case study by PNF program in 4 weeks. Therefore this study will provide a well-planned and structural exercise program for faster improvement in TMD with abnormal neck alignment.
METHODS
Study Design: Parallel, Randomized Controlled Trial, single blinded Sample size of 58, allocation ratio 1:1,
Study Setting: Physiotherapy department, Punjab social security health management company hospital, manga road, raiwind, Lahore.
Recruitment Of Particiants: Fifty eight diagnosed patients of TMD, according to Research Diagnostic Criteria (RDC) of TMD participated. Patient excluded on the base of cervical line angle (CLA<47ᵒ) for FHP 19 and maximum mouth opening <39mm.20 After assessment written informed consent were signed by all participants who were eligible to voluntarily participate in this study.
Sampling Technique: Non probability purposive sampling technique
Sample Selection:
Inclusion Criteria:
Age 20-50 years,
Male and female,
Having temporomandibular joint disorders with abnormal neck alignment,
Pre-diagnosed patients referred by dentist and orthotics.
Exclusion Criteria:
Systemic or local pathology like infectious or vascular disease of orofacial region
Patient using another form of treatment for TMD
Patient using functional appliances
H/o frequent open dislocation
Cervical radiculopathies
Rheumatoid arthritis
Osteoarthritis of TMJ
peripheral nerve injury 21
Diagnosed case of TMD, with FHP and limited mouth opening will be included.
Randomization: Participants will be randomly allocated into two groups. Control group will follow routine physical therapy (RPT) and Experiment group will follow RPT in addition to PNF exercises. Sealed envelope will be used to randomly allocate participant in each groups.
Blinding: This study will be single blinded; senior physiotherapist (assessor) will be blinded to group allocation of participants. Age,gender and BMI was measured on baseline. Pain, ROM and postural alignment will be assessed on baseline, 6th week and follow up on 12th week.
Sample size: The calculated sample size based upon mouth opening which is 24 in each group i.e. n = 48 (24 in each group). By adding 20% drop out rate the final sample size will be 58. i.e. (29 in each group).
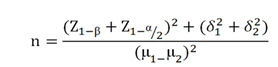
Z1-α/2 Level of significance=95%
Z1-β power of the study= 80%
µ1 Expected mean value of mouth opening with Experimental Group=39.75 (Pilot study)
µ2 Expected mean value of mouth opening with Control Group =37.58 (Pilot study)
δ1 Expected standard deviation in Experimental Group=2.78 (Pilot study)
δ2 Expected standard deviation in Control Group= 2.49 (Pilot study)
n Expected sample size in a group= 29
Outcome Measures
Primary Outcomes:
1. Pain intensity: pain intensity will be assessed by visual analog scale (VAS). Participants choose current pain level after explanation of scale pain levels, which was displayed on Performa from 0 (no pain at all) to 10 (unbearable pain).22,23
2. Range Of Motion: ROM is the extent of movement of a joint, will be measured by vernier caliper.24 TMJ normal ROM is a 40 mm opening, 7 mm lateral deviation, and a 6 mm protrusive movement.20
Secondary Outcomes:
1. Postural assessment: postural alignment will be assessed by CLA for FHP with photogrammetry method. A picture will be taken with digital camera from 2 meters distance. Reflective markers placed on lateral cantus of eye, mid-point of tragus, spinous processof c7 vertebrae and centre of humerus. Lines will be drawn on picture to measure below angles by posture screen app.25,26 Photogrammetry is reliable tool to examine sagittal head, cervical and shoulder angle by a software 27 or mobile app.28 Posture screen app showed good reliability 25 and will be used in this study.
Sagittal head angle (SHA) – The angle between the two line makes SHA. horizontal line passes the tragus and another lateral line that connects the tragus and lateral canthus of eye. 17° angle considered normal.
Cervical line angle (CLA) – The cervical line angle is good and reliable tool to assess FHP. This is the angle also formed by two lines, one horizontal line that cuts through the spinous processes of C7 and another line that connects the tragus. Angle less than 47° considered FHP.
Shoulder angle (SA) – The angle between the center of humerus and the spinous process of C7 formed by two lines called shoulder angle. Angle 51°considered normal.18,27
Ethical considerations: This study is ethically approved IRB-UOL-FAHS/890/2021 6/7/2021 by ethical committee of university of Lahore, Pakistan. After assessment written informed consent will be signed by all participants who were eligible to voluntarily participate in this study. The rules and regulations set by the ethical committee of the University of Lahore will be followed while conducting the research and the rights of the research participants will respected.
· Written informed consent (attached) will be taken from all the participants.
· All information and data collection will be kept confidential.
· Participants will remain anonymous throughout the study.
· The subjects will be informed that there are no disadvantages or risks to the procedure of the study.
· They will also be informed that they will be free to withdraw at any time during the process of the study.
· There will be no known risks associated with this research.
· Their treatment will be giving benefits to the participant; both exercise programs reduce pain and increase range of motion.
· We will do everything we can to protect participant privacy. participant identity will not be revealed in any publication resulting from this study.
· participant participation in this research study is voluntary. participant may choose not to participate and the participant may withdraw their consent to participate at any time. the participant will be penalized in any way, should the participant decide not, participant participate or withdraw from this study.
Data collection procedure: Group A follow routine physiotherapy and group B follow PNF program in addition to routine physiotherapy. Both groups will follow 3 session per week for 4 weeks and home exercises for 2 weeks. pain, range of motion and postural assessment will be conducted on 1st, 6th and 12th week.
Group A
Group A will follow routine physical therapy which include ultrasound/TENS/infrared and ROM/strengthening exercises for 4 weeks (3 session per week).20 Ultrasound therapy (3MHz, 0.8-1.0W/cm2) will be used on TMJ for 4 mins,21 TENS (continuous mode) and infrared lamp will be applied by researcher on temporomandibular joint fo 15 min. Range of motion of TMJ (mouth opening, protrusion and lateral deviation) and static strengthening exercises20 will be advised by researcher. Patient will perform home exercises 3 times a day in 10 repetation.
Group B
Group B will follow routine physiotherapy (TENS/ultrasound/infrared)with PNF program, which is compose of 12 sessions over 4 weeks, each session will continue 30 min and follow home exercise plan for two week. PNF program will be terminated after 4th week.18 Patient will performed PNF program 4 weeks under supervision of therapist or researcher, after 4 weeks follow 2 weeks of home plan.
Proprioceptive neuromuscular facilitation (PNF) programs
The PNF program will compose of a total of eight therapeutic exercises, including the home exercise. In consideration of the alignment of the cervical spine and the pain in the TMJ, the posture with a wider base of support will be modified to have a narrower one. All exercise programs will be designed based on the PNF basic principles, basic procedures, and philosophy of PNF.
The patterns and techniques of PNF will be adapted to the hypothesis of activity limitation. The PNF program, which extends over 4 weeks, took the programs of each week will be adjusted by combining three to four exercise programs. As a result, three sessions will be conducted in each week, and each of these sessions last for 30 min. Before the starting of the exercise program, the patient was given with an overall explanation and detailed instructions on deep-breathing.29 The exercise will be interrupted when the patient reported pain or fatigue to have a 2- to 3-min break. The break will not include in the total duration of exercises.18
Table I: Proprioceptive neuromuscular facilitation (PNF) programs
|
PNF exercise program |
Exercises followed on weekly basis |
|
Contract relax technique used to Elongate extensors of upper cervical. |
1st and 2nd week in hook lying position |
|
Combination of isotonic used for Reciprocal inhibition of sub-occipital muscles with infra-hyoid muscles strengthening |
1st and 2nd week in hook lying position |
|
Stabilizing reversal used in corrected sting posture to increase TMJ ROM with the help of spatula |
1st and 2nd week in sitting position |
|
Combination of isotonics used for tongue exercise in corrected sitting posture of neck |
1st and 2nd week in sitting posture |
|
Approximation applied to Increase mobility of mandible in corrected posture of neck |
2nd week in sitting posture |
|
Combination of isotonics used to improve maximum mouth opening |
3rd and 4th week in sitting posture |
|
Rhythmic stabilization applied with biting a large surface like apple |
4th week in corrected sitting position |
|
Holding the towel behind neck and opening mouth |
2nd, 3rd and 4th week in sitting posture |
Data analysis procedure: SPSS version 21 will be used for data entry and analysis. Quantitative variables will be presented with mean±SD and qualitative variables will be presented with frequency and percentage. Normality of the data will be assessed with Kolmogorov Smirnoff test. If data fulfills the assumption of normality than repeated measure ANOVA will be applied to see the outcome measures (Pain, ROM, Mouth opening, sagittal cervical and shoulder angle) in both treatment groups during course of follow up time duration. In case assumption of normality is violated than alternative non parametric test, man-whitny U test, Friedman test will be applied. p-value <0.05 will be considered statistically significant.
DISCUSSION
This randomized controlled trial addresses the impact of adding PNF to routine physical therapy for TMD in patients with FHP. The study fills a notable gap in existing literature, focusing on the structural implications of FHP on the temporomandibular joint and associated challenges in chewing and eating activities. The choice of PNF as an intervention is well-justified, aligning with its total-body approach and positive outcomes in musculoskeletal diseases with severe pain. The robust methodology, including a blinded assessor and well-defined outcome measures like pain intensity, range of motion, and postural assessment, enhances the study's credibility. The detailed PNF exercise program, rooted in its principles, provides a structured approach to address activity limitations associated with TMD and FHP. If successful, the study has the potential to significantly impact clinical practices, offering an effective exercise plan for TMD patients with abnormal neck alignment.
In conclusion, this article presents a valuable contribution to TMD literature, offering a clear and structured exercise plan for patients with FHP. The study's methodology and rationale for PNF intervention, if proven effective, can inform clinicians and improve the management of TMD, emphasizing the importance of addressing structural issues associated with abnormal neck alignment. The research's ethical considerations and transparent reporting enhance its overall reliability and potential impact on future clinical approaches to TMD.
REFERENCES
1. El Hage Y, Politti F, Herpich CM, de Souza DFM, de Paula Gomes CAF, Amorim CF, de Oliveira Gonzalez T, et al. Effect of facial massage on static balance in individuals with temporomandibular disorder - a pilot study. Int J Ther Massage Bodywork 2013;6(4):6-11. https://doi.org/10.3822/ijtmb.v6i4.208
2. Clark GT, Seligman DA, Solberg WK, Pullinger AG. Guidelines for the examination and diagnosis of temporomandibular disorders. J Craniomandib Disord 1989:3(1):7-14.
3. Key J, Clift A, Condie F, Harley C. A model of movement dysfunction provides a classification system guiding diagnosis and therapeutic care in spinal pain and related musculoskeletal syndromes: a paradigm shift-Part 1. J Bodyw Mov Ther 2008:12(1):7-21. https://doi.org/10.1016/j.jbmt.2007.04.005
4. Morris CE, Greenman PE, Bullock MI, Basmajian JV, Kobesova A. Vladimir Janda, MD, DSc: tribute to a master of rehabilitation. Spine (Phila Pa 1976) 2006;31(9):1060-4. https://doi.org/10.1097/01.brs.0000214879.93102.4e
5. List T, Jensen RH. Temporomandibular disorders: Old ideas and new concepts. Cephalgia 2017;37(7):692-704. https://doi.org/10.1177/0333102416686302
6. Cairns BE. Pathophysiology of TMD pain–basic mechanisms and their implications for pharmacotherapy. J Oral Rehabil 2010;37(6):391-410. https://doi.org/10.1111/j.1365-2842.2010.02074.x
7. Okeson JP. Evolution of occlusion and temporomandibular disorder in orthodontics: Past, present, and future. Am J Orthod Dentofacial Orthop 2015;147(5 Suppl):S216-23. https://doi.org/10.1016/j.ajodo.2015.02.007
8. Cortese S, Mondello A, Galarza R, Biondi A. Postural alterations as a risk factor for temporomandibular disorders. Acta Odontol Latinoam 2017;30(2):57-61.(1852-4834 (Electronic)).
9. Paesani D, Salas E, Martinez A, Isberg A. Prevalence of temporomandibular joint disk displacement in infants and young children. Oral Surg Oral Med Oral Oathol Oral Radiol Endo 1999;87(1):15-9. https://doi.org/10.1016/s1079-2104(99)70288-x
10. De Silveira Coêlho TG, Caracas HM. Perception of the relationship between TMD and orthodontic treatment among orthodontists. Dental Press J Orthod 2015;20(1):45-51. https://doi.org/10.1590/2176-9451.20.1.045-051.oar
11. Rashid A, Matthews NS, Cowgill H. Physiotherapy in the management of disorders of the temporomandibular joint—perceived effectiveness and access to services: a national United Kingdom survey. Br J Oral Maxillofac Surg 2013;51(1):52-7. https://doi.org/10.1016/j.bjoms.2012.03.009
12. De Freitas RF, Ferreira MÂ, Barbosa GA, Calderon PS. Counselling and self-management therapies for temporomandibular disorders: a systematic review. J Oral Rehabil 2013;40(11):864-74. https://doi.org/10.1111/joor.12098
13. Yagi S, Fukuyama E, Soma K. Involvement of sensory input from anterior teeth in deglutitive tongue function. Dysphagia 2008;23(3):221-9. https://doi.org/10.1007/s00455-007-9119-y
14. Kabat H, Knott M. Proprioceptive facilitation technics for treatment of paralysis. Phys Ther Rev 1953;33(3):53-64. https://doi.org/10.1093/ptj/33.2.53
15. Angeli JM, Harpster KL, Hanson E, Sheehan A, Schwab SM. Patient- and caregiver-identified preferences: Dimensions of change in developmental therapy treatment goals. Dev Neurorehabil 2019;22(1):39-46. https://doi.org/10.1080/17518423.2018.1425754
16. Hruby RJ. The total body approach to the osteopathic management of temporomandibular joint dysfunction. J Am Osteopath Assoc 1985;85(8):502-10.
17. Voss DE. Proprioceptive neuromuscular facilitation. Am J Phys Med 1967;4(1):838-99.
18. Lee BK. Influence of proprioceptive neuromuscular facilitation therapeutic exercise on woman with temporomandibular joint disorder: a case study. J Exerc Rehabil 2018;14(6):1074-9. https://doi.org/10.12965/jer.1834406.203
19. Ruivo RM, Pezarat-Correia P, Carita AI. Effects of a resistance and stretching training program on forward head and protracted shoulder posture in adolescents. J Manipulative Physiol Ther 2017;40(1):1-10. https://doi.org/10.1016/j.jmpt.2016.10.005
20. Wright EF, North SL. Management and treatment of temporomandibular disorders: a clinical perspective. J Man Manip Ther 2009;17(4):247-54. https://doi.org/10.1179/106698109791352184
21. Gray D. The relative effectiveness of proprioceptive neuromuscular facilitation versus ultrasound therapy in the treatment of temporamandibular joint dysfunction caused by masticatory myofascial trigger points, in terms of subjective and objective clinical findings 2002. https://doi.org/https://doi.org/10.51415/10321/281
22. Raja SN, Carr DB, Cohen M, Finnerup NB, Flor H, Gibson S, et al. The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain 2020;161(9):1976-82. https://doi.org/10.1097/j.pain.0000000000001939
23. Sung YT, Wu JS. The visual analogue scale for rating, ranking and paired-comparison (VAS-RRP): A new technique for psychological measurement. Behave Res Methods 2018;50(4):1694-1715. https://doi.org/10.3758/s13428-018-1041-8
24. Best N, Best S, Loudovici-Krug D, Smolenski UC. Measurement of mandible movements using a vernier caliper--an evaluation of the intrasession-, intersession- and interobserver reliability. Cranio 2013;31(3):176-80. https://doi.org/10.1179/crn.2013.028
25. Szucs KA, Brown ED. Rater reliability and construct validity of a mobile application for posture analysis. J Phys Ther Sci 2018;30(1):31-6. https://doi.org/10.1589/jpts.30.31
26. van Niekerk SM, Louw Q, Vaughan C, Grimmer-Somers K, Schreve K. Photographic measurement of upper-body sitting posture of high school students: a reliability and validity study. BMC Musculoskelet Disord 2008;9:113. https://doi.org/10.1186/1471-2474-9-113
27. Ruivo RM, Pezarat-Correia P, Carita AI. Intrarater and Interrater Reliability of Photographic Measurement of Upper-Body Standing Posture of Adolescents. J Manipulative Physiol Ther 2015;38(1):74-80. https://doi.org/10.1016/j.jmpt.2014.10.009.
28. Moreira R, Teles A, Fialho R, Baluz R, Santos TC, Goulart-Filho R, et al. Mobile applications for assessing human posture: a systematic literature review. Electronics 2020;9(8):1196. https://doi.org/10.3390/electronics9081196
29. Busch V, Magerl W, Kern U, Haas J, Hajak G, Eichhammer P. The effect of deep and slow breathing on pain perception, autonomic activity, and mood processing--an experimental study. Pain Med 2012;13(2):215-28. https://doi.org/10.1111/j.1526-4637.2011.01243.x
|
Authors declared no conflict of interest
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |