![]() https://doi.org/10.35845/kmuj.2024.23027 ORIGINAL ARTICLE
https://doi.org/10.35845/kmuj.2024.23027 ORIGINAL ARTICLE
Effects of resistive expiratory muscle training onlung functions in patients with chronic obstructive pulmonary disease: a randomized controlled trial
Varda Farooq![]() 1, Muhammad Iqbal Tariq
1, Muhammad Iqbal Tariq![]() 1, Muhammad Fawad
1, Muhammad Fawad![]() 1, Saima Malik
1, Saima Malik![]() 1, Saba Nadeem
1, Saba Nadeem![]() 1, Suman Sheraz
1, Suman Sheraz![]() 1
1
|
1: Riphah College of Rehabilitation & Allied Health Sciences, Islamabad Campus, Riphah International University, Pakistan. 2: Department of Physical Therapy, Faculty of Allied Health Sciences, The Superior University, Lahore, Pakistan
Email
Contact #: +92-307-0509313
Date Submitted: August25, 2022 Date Revised: May 17, 2024 Date Accepted: May27, 2024 |
|
THIS ARTICLE MAY BE CITED AS: Farooq V, Tariq MI, Fawad M, Malik S, Nadeem S, Sheraz S. Effects of resistive expiratory muscle training on lung functions in patients with chronic obstructive pulmonary disease: arandomized controlled trial. Khyber Med Univ J 2024;16(2):110-16. https://doi.org/10.35845/kmuj.2024.23027 |
ABSTRACT
OBJECTIVES: To determine the effects of resistive expiratory muscle training (EMST-150) on lung function, maximum expiratory pressure and quality of life (QoL) in chronic obstructive pulmonary disease (COPD) patients.
METHODS: This randomized controlled trial was conducted on 74 COPD patients, selected through purposive sampling, subsequently randomly assigned to experimental group (n=37) or control group (n=37). Tools used were digital spirometer for forced expiratory volume in 1 second (FEV1), forced vital capacity (FVC), peak expiratory flow (PEF), Dyspnea grade was calculated using Borg scale and QoL was measured using St. George's Respiratory Questionnaire (SQRG) supervised twice in people with COPD. Baseline data were taken at week-1 before the training and at the completion of the study which was at 6th week.
RESULTS: Post-treatment, Experimental Group demonstrated a significant increase in FEV1 compared to Control Group (2.15±0.12 vs. 1.91±0.17, p<0.001). There was a significant difference in FVC between Experimental Group and Control Group after six weeks of treatment (2.26±0.12 vs. 1.96±0.21, p<0.001). No significant difference in PEF was observed between two groups, either before (p = 0.372) or after (p = 0.279) treatment.Regarding QoLfor Experimental and Control groups, pre-training SQRG score (Median-Interquartile range) was 55.47 (14.58) and 55.72 (10.435) respectively (p=0.520) and post-training SQRG score was 15.76 (6.875) and 23.91 (6.625) respectively (p<0.001).
CONCLUSION: EMST-150 is an effective and beneficial intervention for enhancing lung functions and improved QoL in patients with COPD. These results highlight the potential benefits of incorporating EMST-150 into respiratory rehabilitation programs for individuals with respiratory conditions.
Clinical Trial Registration Number: NCT05061186
KEYWORDS: Pulmonary Disease, Chronic Obstructive (MeSH); Diaphragmatic Breathing (Non-MeSH);Respiration (MeSH); EMST-150 (Non-MeSH); Incentive Spirometer (Non-MeSH); Spirometry (MeSH); Pulmonary Rehabilitation (Non-MeSH); Rehabilitation (MeSH); Pursed Lip Breathing (Non-MeSH); Quality of Life (MeSH).
INTRODUCTION
Chronic obstructive pulmonary disease (COPD) is a global health issue affecting 10% of the adult population, with its incidence rising due to an ageing population.1 COPD is characterized by airway restriction and an inappropriate immune response. The Global Initiative for Chronic Obstructive Lung Disease (GOLD) classification system, based on post-bronchodilator spirometry, is widely used to assess COPD severity. A diagnosis of COPD is confirmed with a forced expiratory volume in one second (FEV1) to forced vital capacity (FVC) ratio of less than 0.7.2
Researchers have explored various methods to improve respiratory function in COPD patients, particularly those with dysphagia. One promising method is expiratory muscle strength training (EMST), which has been shown to enhance breathing function.3 EMST has demonstrated benefits in improving the voluntary cough reflex and managing dysphagia in conditions such as central nervous system illnesses that cause muscle weakness, potentially leading to restricted respiratory flow similar to COPD.4 Studies indicate that EMST programs can increase maximum expiratory pressure (PE max) and improve speech, swallowing, respiration, and physical performance, suggesting EMST as a therapeutic approach for voice impairments or dysphagia. However, further research focusing on task-specific exercise programs is needed.4\
EMST has also been found to reduce breathlessness during physical activities and increase walk able distance in both healthy individuals and COPD patients.5,6Additionally, research has demonstrated aerodynamic improvements in cough airflow characteristics in multiple sclerosis (MS) patients, the elderly, and those with Parkinson's disease (PD); improved swallow safety in PD patients; and post-EMST variations in voice aerodynamic and auditory parameters in PD patients.4
Crisafulli E, et al., found that repetitive muscle training (RMT) is superior to inspiratory muscle training (IMST) in reducing dyspnea in COPD patients.7 They suggest a trial combining IMST and EMST in COPD patients to evaluate the physiological benefits and exhalation forces of the combined workout.8 There is limited research on expiratory muscle training (EMT), but it has been suggested to strengthen inhalation and exhalation muscles alone or in combination with IMST in COPD patients. The long-term effects of this training, however, remain unknown.9
A study supports EMST as a treatment for dysphagia in COPD patients, showing improvements in dyspnea and highlighting the need for alternative treatments. Combining EMST and IMST showed improvement after 6-12 months, with findings varying depending on COPD severity.10 EMST focuses on strengthening the respiratory muscles, which are rarely subjected to vigorous exercise. However, there has been insufficient research to determine the true benefits of muscle strength training on breathing, coughing, swallowing, and
A 2023 pilot study demonstrated that using EMST-150 with pursed lip breathing significantly enhanced outcomes in COVID-recovered patients, especially at higher resistance levels (p<0.001).11 This study was planned to assess the effects of EMST-150 in managing COPD, addressing a significant gap in the literature and elucidating its therapeutic benefits. This research explores the relatively unexamined area of resistive expiratory muscle strength training and its impact on pulmonary function, providing valuable insights into its potential to improve pulmonary metrics and quality of life in COPD patients. Building on previous research, this investigation utilizes the EMST-150 device for mild resistive training, focusing on its effects on pulmonary function and expiratory pressure.
METHODS
This randomized controlled trial was conducted at Holy Family Hospital Rawalpindi, Pakistan, from July to December 2021. Ethical approval was obtained from Riphah International University (Ethical number: RIPHAH/FR&AHS/Letter-0870) and the trial was registered with ClinicalTrials.gov under registration number NCT05061186.
The study used a non-probability convenience sampling method to select patients, and informed consent was obtained from each participant before enrollment. Ninety-five patients were initially assessed, with 74 meeting the inclusion criteria. The study included patients of both genders, aged between 40 and 75 years, diagnosed with dyspnea (Borg scale ≤4) and moderate to moderately severe COPD according to GOLD criteria. Exclusion criteria comprised patients with orthopedic conditions, neurological illness, impaired cognition (Mini-Mental State Examination <22), heart problems, acute or chronic infections, lung fibrosis, or obstructive sleep apnea syndrome (OSAS).
The 74 eligible individuals were randomly assigned to two groups using a lottery method. Details regarding enrollment, intervention allocation, follow-up, and data analysis are provided in Figure 1.
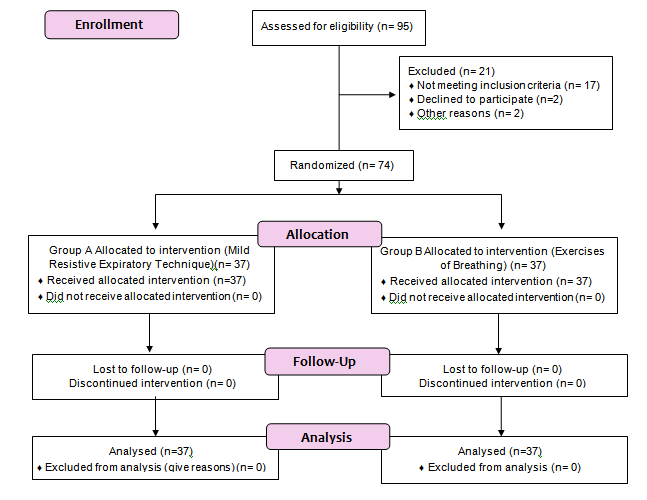
Figure 1: CONSORT flow Diagram
Group A received intervention using the Expiratory Muscle Strength Training (EMST150) device for respiratory muscles (Figure 2).

Figure 2: Expiratory Muscle Strength Training (EMST-150)
This intervention involved Mild Resistive Expiratory Technique sessions from the EMST150 device. Group B received Breathing Exercises as their intervention. Both interventions were administered 5 days a week for a total duration of 6 weeks Table 1.
Table I: Detail Intervention Protocol
|
|
Interventional group |
Control group |
|
Week 1 to 6 |
Mild Resistive Expiratory Technique (EMST150 is a 6-week training routine that takes about 20 minutes/day) The EMST participant must exhale for five seconds into the equipment with plenty of effort to open the one-way valve. A single repeat represented by each "blow." The resistance of the device was set to 30 cmH2O. On any five days of the week, participants were requested to perform for 6 weeks, do 5 sets of 5 reps (a maximum of 25 times and about twenty minutes every day).The task was completed entirely while seated. Depending on the patient's comfort level, rest was given between repetitions.
|
Exercises of Breathing: (approximately twenty minutes/day) 2 Breathing via pursed lips: (In your armchair, erect your spine. Breathe in deeply for 2 seconds via your nostrils. Breathe out gently for twice as much time as you breathed in, pursing your lips as if you were blowing on meals. at least 4 to 5 times per day) ● Diaphragmatic breathing: (Entirely flat on the floor with your knees bent and your head supported.) To support your legs, place a pillow under your knees. Slowly inhale through your nose. Exhale through pursed lips while tightening your stomach muscles and letting them fall inward. 3-4 times every day, do this work out for 5-10 minutes). ● Incentive spirometer: (Maintain a standing position. Slowly and deeply inhale as much as you can. Breathe deeply and hold it for as much as you can (for at least five sec.). Expire gradually after that. Every hour, relax for just few seconds and then at least 10 times). |
The data were analyzed using SPSS version 21. The data from the Spirometer like forced expiratory volume in one second (FEV1); forced vital capacity (FVC) and peak expiratory flow rate (PEF) were assessed for normality using the Shapiro-Wilk test. Since these variables showed normal distribution, parametric tests were applied. Non-parametric tests were used for variables that did not exhibit normal distribution. Between-group analyses utilized the Independent t-test and Mann Whitney U-test, while within-group analyses employed the Paired t-test and Wilcoxon test. The significance level was set at p < 0.05.
RESULTS
Out of 74 patients with moderately severe COPD, the experimental group comprised 30 males and 7 females, while the control group included 31 males and 6 females. The mean age of the experimental group and control group was 53.08±4.41 and 55.48±6.19years respectively.
Independent t-tests were applied for FEV1 and FVC. The mean ± SD values of FEV1 and FVC for the experimental group before training were 1.51 ± 0.11 and 1.58 ± 0.14, respectively, and for the control group were 1.40 ± 0.12 and 1.56 ± 0.13, respectively. After training, these values for the experimental group were 1.61 ± 0.11 and 1.69 ± 0.14, and for the control group were 1.50 ± 0.11 and 1.46 ± 0.15, respectively.
Significant differences (p < 0.05) were found for FEV1 and FVC except at baseline. PEF analysis using independent t-tests showed non-significant p-values (> 0.05), specifically 0.372 for the first week and 0.279 for the sixth week (Table II).
Table II: Comparison of Pulmonary Function Parameters (FEV1, FVC, PEFR) in Experimental and Control Groups Before and After Training
|
Experimental/Control and Pre/ post groups |
Week-1 Mean ±SD |
Week-2 Mean±SD |
Week-3 Mean±SD |
Week-4 Mean±SD |
Week-5 Mean±SD |
Week-6 Mean±SD |
|
|
FEV1 (L) |
Experimental group pre training |
1.05±0.07 |
1.24±0.93 |
1.40±0.12 |
1.54±0.11 |
1.78±0.13 |
2.01±0.13 |
|
Control group pre training |
1.07±0.11 |
1.20±0.10 |
1.32±0.09 |
1.46±0.09 |
1.59±0.16 |
1.78±0.17 |
|
|
P value pre training |
0.452 |
0.066 |
0.003 |
<0.001 |
<0.001 |
<0.001 |
|
|
Experimental group post training |
1.16±0.08 |
1.34±0.10 |
1.49±0.11 |
1.65±0.12 |
1.89±0.15 |
2.15±0.12 |
|
|
Control group post training |
1.14±0.07 |
1.28±0.09 |
1.40±0.08 |
1.54±0.08 |
1.70±0.15 |
1.91±0.17 |
|
|
P-value post training |
0.346 |
0.017 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
|
|
FVC(L) |
Experimental group pre training |
1.08±0.07 |
1.33±0.17 |
1.46±0.13 |
1.61±0.14 |
1.88±0.21 |
2.10±0.13 |
|
Control group pre training |
1.09±0.08 |
1.24±0.10 |
1.38±0.10 |
1.53±0.15 |
1.65±0.15 |
1.85±0.20 |
|
|
P value pre training |
0.733 |
0.009 |
0.003 |
0.023 |
<0.001 |
<0.001 |
|
|
Experimental group post training |
1.19±0.08 |
1.44±0.24 |
1.54±0.11 |
1.76±0.17 |
1.96±0.14 |
2.26±0.12 |
|
|
Control group post training |
1.18±0.09 |
1.33±0.09 |
1.46±0.11 |
1.61±0.17 |
1.80±0.22 |
1.96±0.21 |
|
|
P value post training |
0.543 |
0.010 |
0.005 |
<0.001 |
<0.001 |
<0.001 |
|
|
PEFR (L/min) |
P value pre training |
0.372 |
|
|
|
|
|
|
P value post training |
|
|
|
|
|
0.279 |
|
FEV1: Forced Expiratory Volume in one second; FVC: Forced Vital Capacity; PEF:Peak Expiratory flow rate, L=Litres; Independent T test was used for data analysis
The Mann-Whitney U test was applied to evaluate MEP, incentive spirometer, and Borg scale scores. In the experimental group, the median and interquartile ranges (IQ) pre-training, including the baseline average, were 45.84 (5), 1633.4 (616.7), and 1.584 (0.917), respectively. Post-training values were 50.84 (6.67), 2200 (583.4), and 1 (0.584). For the control group, pre-training medians were 39.17 (7.5), 1166.7 (308.4), and 1.75 (0.84), while post-training medians were 37.5 (9.17), 1450 (433.4), and 1.25 (0.34). The p-values for MEP and incentive spirometry were significant (p < 0.05), except for the baseline value. For the Borg scale score, p-values for the first week and post-training at the 4th and 5th weeks were greater than 0.05, while all others were significant (p < 0.05). The p-value for the St. George's Questionnaire was < 0.01 (Table III).
Table III: Comparison of Respiratory and Quality of Life Parameters Before and After Training with EMST and Incentive Spirometry in Experimental and Control Groups
|
Experimental/controlgroups (Pre/ post training) |
Week1 Median(IQ) |
Week2 Median(IQ) |
Week 3 Median(IQ) |
Week 4 Median(IQ) |
Week 5 Median(IQ) |
Week 6 Median(IQ) |
|
|
MEP |
Experimental group pre-training |
30(5) |
45(5) |
55(5) |
35(5) |
50(5) |
60(5) |
|
Control group pre-training |
30(0) |
35(10) |
45(12.5) |
35(0) |
40(0) |
50(12.5) |
|
|
P value pre-training |
0.095 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
|
|
Experimental group post training |
35(5) |
50(5) |
60(7.5) |
40(5) |
55(5) |
65(12.5) |
|
|
Control group post-training |
30(5) |
35(10) |
40(12.5) |
35(5) |
40(10) |
45(12.5) |
|
|
P value post-training |
0.035 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
|
|
Incentive spirometery |
Experimental group pre-training |
300 (200) |
1500 (750) |
2500 (900) |
700 (400) |
1800 (550) |
3000 (900) |
|
Control group pre-training |
300 (250) |
1000 (150) |
1700 (500) |
500 (250) |
1200 (200) |
2000 (500) |
|
|
P value pre-training |
0.064 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
|
|
Experimental group post-training |
1000 (350) |
2000 (800) |
3000 (950) |
1200 (500) |
2500 (800) |
3500 (1000) |
|
|
Control group post-training |
500 (200) |
1300 (350) |
2100 (700) |
800 (200) |
1500 (400) |
2500 (750) |
|
|
P value post-training |
0.002 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
|
|
Borg scale score |
Experimental group pre-training |
3.000 (2.000) |
2.00 (1.00) |
1.00 (0.50) |
2.00 (1.00) |
1.00 (0.50) |
0.50 (0.50) |
|
Control group pre-training |
3 (1) |
2 (1) |
1 (0.50) |
3 (1) |
1 (1) |
0.50 (0.50) |
|
|
P value pre-training |
0.054 |
0.008 |
0.002 |
0.010 |
0.012 |
0.002 |
|
|
Experimental group post-training |
3.000 (1.000) |
0.50 (0.50) |
0.00 (0.50) |
2.00 (1.00) |
0.50 (0.50) |
0.00 (0.00) |
|
|
Control group post-training |
3 (0) |
1 (1) |
0.50 (0) |
2 (0) |
0.50 (0.50) |
0.50 (0.50) |
|
|
P value post-training |
0.119 |
0.017 |
0.024 |
0.184 |
0.236 |
0.001 |
|
|
St. George Questionanaire |
Experimental group pre-training |
55.47 (14.58) |
|
|
|
|
|
|
Control group pre training |
55.72 (10.435) |
|
|
|
|
|
|
|
P value pre-training |
0.520 |
|
|
|
|
|
|
|
Experimental group post-training |
|
|
|
|
|
15.76 (6.875) |
|
|
Control group post-training |
|
|
|
|
|
23.91 (6.625) |
|
|
P value post-training |
|
|
|
|
|
<0.001 |
|
MEP: Maximum Expiratory Pressure; Mann-Whitney U test was used for data analysis
Among Experimental Group and Control Group, there is statistical significant difference with p value <0.001, when we applied within group analysis on each variable (FEV1, FVC, PEF, MEP, IS)
DISCUSSION
Our study on the effects of resistive expiratory muscle training through EMST-150 device in COPD patients demonstrated statistically significant improvements (p <0.001) in lung function parameters FEV1, FVC, PEF, MEP, and quality of life measures compared to controls. These findings highlight the efficacy of resistive expiratory muscle training in enhancing respiratory function and overall well-being among individuals with moderately severe COPD. In the previous studies, Nield Mokhlasi B, et al.,12 concluded that while an EMST group showed reduced exceptional dyspnea, pursed lip breathing was deemed the most effective treatment. However, their study focused on prolonging expiration rather than specifically strengthening expiratory muscles. Conversely, de Deus CR, et al.,13 found that all treatment groups demonstrated improvement, with the most significant benefits observed in the group undergoing respiratory physiotherapy combined with IMST and EMST.
In our current study, there was no improvement in PEF observed in either of the two groups. This contrasts with previous studies that reported significant improvements in PEF, potentially due to longer intervention periods and larger sample sizes than those in our study. However, we found that FEV1 improved significantly after six weeks of training in both groups. This aligns with findings by Mota S, et al.,5 who observed increased lung volume and enhanced cough effectiveness, which are crucial for airway protection.
In previous randomized controlled trials and a meta-analysis, muscle endurance training focused on 30-minute sessions at 50-60% of MEP.15,16 Weiner P, et al.,15 extended this training period to 12 weeks in COPD patients. In Temple man’s systematic review,16 the Forrest plots showed high homogeneity between studies (I²=0%). The meta-analysis revealed that EMST led to a significant improvement in MEP compared to control groups, with a standardized mean difference of 19.93 cmHO (95% CI: 8.88 to 30.97; p=0.0004).Similarly, our present study also shows a significant improvement in MEP among COPD patients using EMST, with a p-value of <0.001.
The difference with the present study is due to the different population; they included all stages of COPD patients, while the present study only included moderate and moderately severe stage COPD patients. Additionally, the study duration was different, being 12 weeks.15 According to a previous study by Ozan Kacmaz, et al.,17 the use of an incentive spirometer in patients with COPD is effective and significant, with a p-value of <0.001 compared to medical treatment alone. The present study supports these results, showing a significant difference in the use of incentive spirometer (p < 0.001).
Both groups initially showed no significant differences at baseline, but from the first week to the sixth week, both exhibited marked improvements with a p-value of <0.001 at the sixth week. This finding is supported by a randomized controlled trial conducted in 2018 by Zoe McKeough and colleagues.18 In their study, they investigated the impact of an eight-week short-form Sun-style Tai Chi program on physical activity, exercise capacity, and quality of life in individuals with COPD. The results indicated a lower The St. George's Respiratory Questionnaire (SQRG) score, indicating better quality of life, although there was no observed improvement in activity levels.
In the current study, a significant difference was observed in The Medical Research Council (MRC) scores for both groups (p =0.001). When comparing baseline scores between the groups, the experimental group showed clinically meaningful improvements starting from week-3, which continued through week-6. These findings suggest that if this program is extended over a longer duration, it could lead to more pronounced positive changes. In a previous study,19 no systematic changes over time were found in the slope of any of the Borg/objective index relationships. Additionally, studies by Cvejic et al.,20 and Gross RD, et al.21have shown improvements in dyspnea, strength, and exercise performance through EMST and combined EMST plus IMST training.
The study assessed only a few pulmonary function variables due to budget constraints and equipment limitations. Future research should include additional variables such as functional residual capacity, residual volume, and expiratory reserve volume. Moreover, longer follow-up periods should be considered to better understand the effects over time.
Exploring EMST across various neurological disorders could uncover cross-benefits on swallow impairment, lung function, airway protection, and disease severity or progression. This investigation may reveal the long-term efficacy of EMST in these areas.
CONCLUSION The study found significant improvements in FEV1, FVC, MEP, incentive spirometry, and Borg scale scores in both groups. However, resistive expiratory muscle training (EMST-150) showed superior efficacy in enhancing respiratory parameters. Both groups also exhibited significant improvements in quality of life, as indicated by scores on the St. George's questionnaire. These results highlight the potential benefits of incorporating EMST-150 into respiratory rehabilitation programs for individuals with respiratory conditions.
ACKNOWLEDGMENT We acknowledge the contributions of Dr. Khurram (Head of Medical Unit 2, Holy Family Hospital, Rawalpindi), Mr. Yousaf Burki, Dr. Mehwish Waseem, and the staff of the Post Graduate Laboratory at Riphah International University. Their efforts in patient recruitment, data collection, manuscript writing, and provision of the EMST-150 and Incentive Spirometer are greatly appreciated.
REFERENCES
1. Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 2007;176:532-55. https://doi.org/10.1164/rccm.201204-0596PP
2. Kim J, Sapienza CM. Implications of expiratory muscle strength training for rehabilitation of the elderly: Tutorial. J Rehabil Res Dev 2005;42(2):211-24. https://doi.org/10.1682/jrrd.2004.07.0077
3. Neves LF, Reis MH, Plentz RD, Matte DL, Coronel CC, Sbruzzi G. Expiratory and expiratory plus inspiratory muscle training improves respiratory muscle strength in subjects with COPD: systematic review. Respir Care 2014;59(9):1381-8. https://doi.org/10.4187/respcare.02793
4. Laciuga H, Rosenbek JC, Davenport PW, Sapienza CM. Functional outcomes associated with expiratory muscle strength training: narrative review. J Rehabil Res Dev 2014;51(4):535-46. https://doi.org/10.1682/JRRD.2013.03.0076
5. Mota S, Güell R, Barreiro E, Solanes I, Ramírez-Sarmiento A, Orozco-Levi M, et al. Clinical outcomes of expiratory muscle training in severe COPD patients. Respir Med 2007;101(3):516-24. https://doi.org/10.1016/j.rmed.2006.06.024
6. Suzuki S, Sato M, Okubo T. Expiratory muscle training and sensation of respiratory effort during exercise in normal subjects. Thorax 1995;50(4):366-70. http://doi.org/10.1136/thx.50.4.366
7. Crisafulli E, Costi S, Fabbri LM, Clini EM. Respiratory muscles training in COPD patients. Int J Chron Obstruct Pulmon Dis 2007;2(1):19-25. http://doi.org/10.2147/copd.2007.2.1.19
8. Sapienza CM. Respiratory muscle strength training applications. Curr Opin Otolaryngol Head Neck Surg 2008;16(3):216-20. http://doi.org/10.1097/MOO.0b013e3282fe96bd
9. Xu W, Li R, Guan L, Wang K, Hu Y, Xu L, et al. Combination of inspiratory and expiratory muscle training in same respiratory cycle versus different cycles in COPD patients: a randomized trial. Respir Res 2018;19(1):225. http://doi.org/10.1186/s12931-018-0917-6.
10. Cvejic L, Harding R, Churchward T, Turton A, Finlay P, Massey D, et al. Laryngeal penetration and aspiration in individuals with stable COPD. Respirol 2011;16(2):269-75. http://doi.org/10.1111/j.1440-1843.2010.01875.x.
11. Morgan S, Visovsky C, Thomas B, Klein AB, Ji M, Schwab L, Coury J, et al. Home-Based Pilot Pulmonary Program for Dyspneic Patients Post-COVID-19. Clin Nurs Res 2023;32(5):895-901. https://doi.org/10.1177/10547738231170496
12. Mokhlesi B, Logemann JA, Rademaker AW, Stangl CA, Corbridge TC. Oropharyngeal deglutition in stable COPD. Chest 2002;121(2):361-9. http://doi.org/10.1378/chest.121.2.361
13. de Deus CR,, Carvalho CR, Cukier A, Stelmach R, Andrade CR. Symptoms of dysphagia in patients with COPD. J Bras Pneumol 2011;37(2):176-83. http://doi.org/10.1590/s1806-37132011000200007
14. Clayton NA, Carnaby GD, Peters MJ, Ing AJ. Impaired laryngopharyngeal sensitivity in patients with COPD: the association with swallow function. Int J Speech Lang Pathol 2014;16(6):615-23. http://doi.org/10.3109/17549507.2014.882987.
15. Weiner P, Magadle R, Beckerman M, Weiner M, Berar-Yanay N. Specific expiratory muscle training in COPD. Chest 2003;124(2):468-73. http://doi.org/10.1378/chest.124.2.468
16. Templeman L, Roberts F. Effectiveness of expiratory muscle strength training on expiratory strength, pulmonary function and cough in the adult population: a systematic review. Physiotherapy 2020;106:43-51. http://doi.org/10.1016/j.physio.2019.06.002
17. Basoglu OK, Atasever A, Bacakoglu F. The efficacy of incentive spirometry in patients with COPD. Respirol 2005;10(3):349-53.http://doi.org/10.1111/j.1440-1843.2005.00716.x
18. McKeough Z, Leung R, Wootton S, Cheng S, Alison J. Effect of short form, sun-style tai chi on physical activity in people with COPD. Eur Respir J 2013;41(5):1051-7; https://doi.org/10.1183/13993003.congress-2018.PA5423
19. Mador MJ, Rodis A, Magalang UJ. Reproducibility of Borg scale measurements of dyspnea during exercise in patients with COPD. Chest 1995;107(6):1590-7. https://doi.org/10.1378/chest.107.6.1590
20. Cvejic L, Harding R, Churchward T, Turton A, Finlay P, Massey D,et al. Laryngeal penetration and aspiration in individuals with stable COPD. Respirol 2011;16(2):269-75. https://doi.org/10.1111/j.1440-1843.2010.01875.x
21. Gross RD, Atwood CW Jr, Ross SB, Olszewski JW, Eichhorn KA. The coordination of breathing and swallowing in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2009;179(7):559-65. https://doi.org/10.1164/rccm.200807-1139OC
|
CONFLICT OF INTEREST Authors declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work. GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |