![]() https://doi.org/10.35845/kmuj.2023.22993 VIEW
POINT
https://doi.org/10.35845/kmuj.2023.22993 VIEW
POINT
UTILITY OF SPIROMETRY IN ASSESSMENT OF UPPER AIRWAY OBSTRUCTIONSt HE NEGLECTED PARAMETERS
Thamir al-Khlaiwi 1 ,
Syed Shahid Habib 1
,
Syed Shahid Habib 1
|
1: Department of Physiology, College of Medicine, King Saud University, Riyadh, Kingdom of Saudi Arabia
Email Contact #: +966-053260078 Date Submitted: July 22, 2022 Date Revised: January 25, 2023 Date Accepted: January 26, 2023 |
|
THIS ARTICLE MAY BE CITED AS: Al-Khlaiwi T, Habib SS. Utility of spirometry in assessment of upper airway obstructions: the neglected parameters. Khyber Med Univ J 2023;15(1):60-5. https://doi.org/10.35845/kmuj.2023.22993 |
ABSTRACT
Upper airway obstructions represent a huge burden to the health care system due to its high morbidity and cost to the economic systems. Therefore, it is important to understand the physiological parameters used in diagnosis and prognosis of these diseases. Various physiological lung parameters should be examined simultaneously to make the precise diagnosis of upper airway obstruction. Relying on only one parameter and neglecting others might lead to misdiagnosis and subsequent mismanagement. The shape of the flow-volume loop, Forced Expiratory Flow at 50% of vital capacity/Forced Inspiratory Flow at 50% of vital capacity ratio (FEF-50%/FIF-50%), Forced Expiratory Volume in 1 second /Forced Expiratory Volume after 0.5 seconds (FEV1/FEV0.5), Empey index, and the refined version of the Expiratory Disproportion Index (EDI) are of great value in the diagnosis of different types of upper airway obstructions. The shape of the flow-volume loop changes earlier than other spirometrical parameters and is very useful in detecting early changes in upper airway diseases. This review was aimed to explain and simplify the role of pulmonary function tests and flow volume curve not only for pulmonologists, but also for surgeons, anesthesiologists, and ENT specialists who can utilize and implement usefully these tests in their clinical practice.
KEYWORDS: Airway Obstruction (MeSH);Pulmonary Disease, Chronic Obstructive (MeSH); Diagnosis (MeSH);Respiratory Function Tests (MeSH); Spirometry (MeSH);Forced Expiratory Volume(MeSH);Forced Expiratory Flow Rates(MeSH);FEF50%/FIF50% (Non-MeSH);FEV1/FEV0.5(Non-MeSH).
INTRODUCTION
Upper airway obstructions represent a huge burden to health care system due to its high mortality and morbidity whether it is acute or chronic. Upper airway obstructions can be defined as decrease in diameter of the larynx, extrathoracic or intrathoracic trachea, and main bronchi.1Three types of abnormalities have been observed in upper airway obstruction:
(1) Variable intrathoracic obstructions: In variable obstructions, the diameter of the airway changes according to the change in transmural pressure during inspiration and expiration. The patient experiences reduced forced expiration, while the inspiration remains normal. There are several causes of variable intrathoracic obstructions which include tumors of the lower trachea, main stem bronchus, and tracheomalacia.1
(2) Variable extrathoracic obstructions: The patient experiences reduced forced inspiration with normal expiration. Some causes of variable extrathoracic obstructions include vocal cord dysfunction, laryngeal edema, and laryngeal tumors.1
(3) Fixed upper airway obstructions: The diameter of the airway does not change with the change in transmural pressure during inspiration and expiration. Fixed intrathoracic and extrathoracic airway obstructions lead to decrease air flow during inspiration and expiration, irrespective of the site of obstruction.1 Some causes of fixed upper airway obstructions include goiter`s, and post-intubation stenosis.
SPIROMETRY PARAMETERS
Besidemedical history of the patient and radiological imaging, spirometry can be used to assure precise diagnosis. Patient usually is asymptomatic unless airways are significantly reduced. Resting dyspnea usually appears if the diameter of airway is reduced to 5 mm while dyspnea with physical activity appearsif the diameter of the airway is reduced to 8 mm.2In this regard, it is very important to take into consideration that narrowing of the airway has to be around 80 % to be detected by spirometryif we take other factors into account such as age, gender, and BMI.1,3In addition, forced expiratory volume in one second (FEV1) remains above 90% if the tracheal diameter is >6 mm.4One difference between upper airway obstruction and lower airway obstruction (restrictive and obstructive disorders) in spirometry findings is that the forced expiratory volume in one second (FEV1) is usually the least affected or almost normal in upper airway obstruction.1
It has been found that maximal voluntary ventilation (MVV)and Peak Expiratory Flow Rate (PEFR) are more reliable parameters to detect mild and moderate upper airway obstruction. If the ratio of MVV to FEV1 (MVV/FEV1) <25%, upper airway obstruction is usually suspected.5
THE SHAPE OF FLOW-VOLUME LOOP (FVL):
FVL is critical in evaluation of the abnormalities of upper airway obstruction, location of the obstruction (intrathoracic or extrathoracic), severity, and treatment effectiveness.3 FVL is created by plotting maximal inspiratory and expiratory flows against the lung volume. The shape of the FVL changes earlier than spirometry parameters.5In upper airway obstruction, patients are presented with three different FVL shapes (Figure 1).
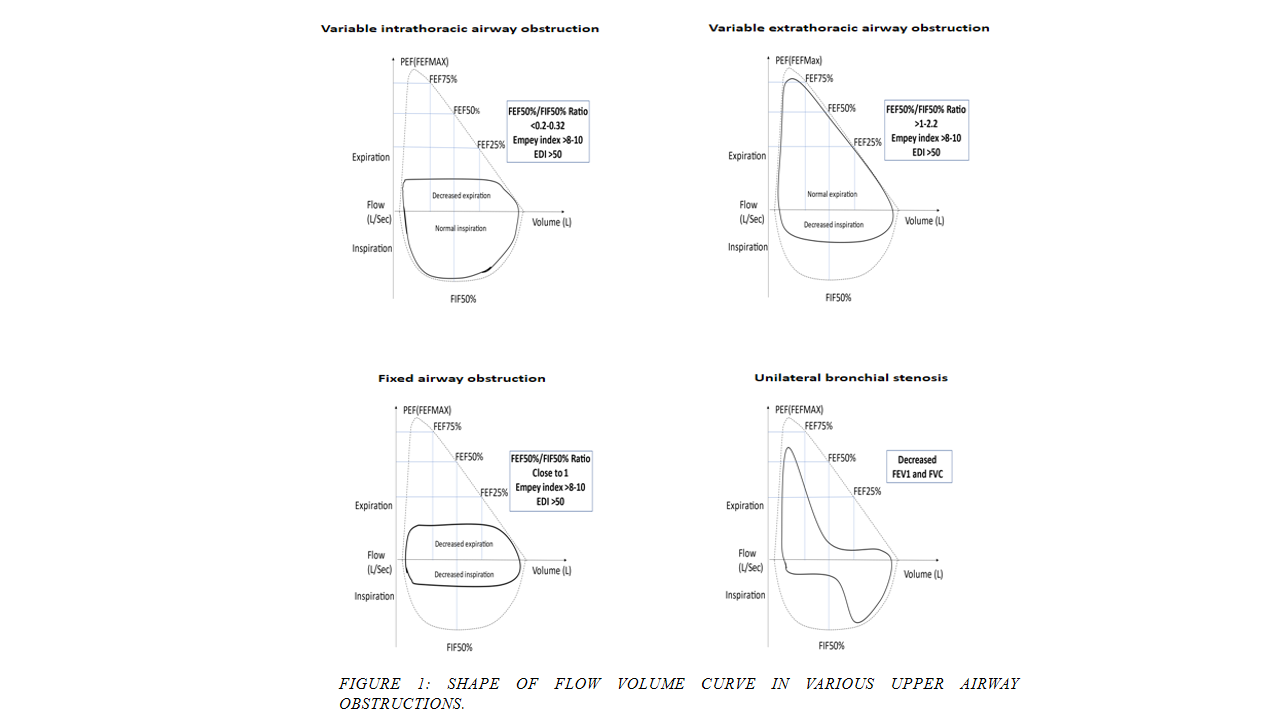
Notes: Dashed lines represent normal flow volume curve. Solid lines represent abnormal flow volume curve.
Flow-volume loop in variable intrathoracic upper airway obstruction:
It shows limitation of maximal expiratory flow (“clipping” of the expiratory FVL) while the inspiratory side of the loop is normal (Figure 1). In this situation, the intrapleural pressure becomes positive resulting in an increase surrounding pressure which compresses the affected airways. When the patient expires forcefully, the pressure surrounding the intrathoracic airway becomes larger than the intratracheal pressure, leading to airway collapse and thus obstruction. However, when the patient inspiresforcefully, the intratracheal pressure becomes greater than the surrounding pressure, which leads to normal inspiration.6 For example, an intrathoracic mass (tumor),located around outer upper airwaystructures, produces a normal inspiratory side of the FVL due to increased negativity of intrathoracic pressure during inhalationand a flattened expiratory side of the FVL due to the obstruction of the trachea.7
Flow-volume loop in variable extrathoracic upper airway obstruction:
It shows limitation of maximal inspiratory flow (“clipping” of the inspiratory FVL), with a normal expiratory side of the loop (Figure 1). When the patient is forcefully expiring, the extrathoracic pressure will be less than the intratracheal pressure, which results in normal expiration. During inspiration, the extrathoracic pressure is greater than the intratracheal pressure, which leads to reduced inspiration and thus obstruction.6
Flow-volume loop in fixed extrathoracic upper airway obstruction:
It shows limitation of both maximal inspiratory and expiratory flow rates (“clipping” of the inspiratory and expiratory sides of the FVL) (Figure 1). Changes in transmural pressure do not affect the airway during inspiration and expiration. A mass compressing the trachea (e.g., goiter or lymphoma) or laryngotracheal stenosiscould produce this pattern. Strong associations were found between Total Peak Flow[Peak Expiratory Flow (PEF) + Peak Inspiratory Flow (PIF)],8 PEF, Expiratory Disproportion Index(EDI)9and the changes noted postoperatively with a successful surgery.
FEF-50/FIF-50 RATIO:
In normal situations, forced inspiratory flow is effort-dependent, while forced expiratory flow is effort-independent during almost 80% of the maximal expiratory flow.Consequently, the mid-inspiratory flow measured at 50% of the FVC (FIF50% or MIF50%) is higher than the maximal expiratory flow at 50% of FVC (FEF50% or MEF50%).10Therefore, in normal situations: FEF50%/FIF50% ratio <1. In variable intrathoracic upper airway obstruction, the ratio is <0.2-0.32 as for example in intraluminal tumors involving the lower trachea, or tracheomalacia. In variable extrathoracic upper airway obstruction, the ratio is >1-2.20 as for examplein vocal cord dysfunction, vocal cord paralysis, or edema. In fixed upper airway obstructions (intrathoracic or extrathoracic), the ratio of FEF50%/FIF50% is close to 1.5
THE EMPEY INDEX:
Empey index is measured byFEV1 (ml/s) divided by PEF (l/min). Empey index values >8-10 are considered to be abnormal.11 FEV1/PEF ratio has been well established index in the diagnosis of upper airway obstructions.12,13
The refined version of the Empey index is called the “Expiratory Disproportion Index” (EDI= FEV1 [L]/PEFR [L−S] × 100). At a threshold of >50, EDI is highly sensitive for diagnosing upper airway obstructions.14 Table 1 shows summary of functional parameters in upper airway obstruction.
Table I: SUMMARY OF FUNCTIONAL PARAMETERS IN UPPER AIRWAY OBSTRUCTION
|
Functional Parameters |
Variable intrathoracic airway obstruction |
Variable extrathoracic airway obstruction |
Fixed airway obstruction |
|
Maximum expiration |
Decreased |
Normal |
Decreased |
|
Maximum inspiration |
Normal |
Decreased |
Decreased |
|
FEV1 |
Least affected or normal |
Least affected or normal |
Least affected or normal |
|
Expiratory Curve |
Limited |
Normal |
Limited |
|
Inspiratory Curve |
Normal |
Limited |
Limited |
|
FEF50%/FIF50% Ratio |
<0.2-0.32 |
>1-2.2 |
Close to 1 |
|
Empey index: FEV1/PEF |
>8-10 |
>8-10 |
>8-10 |
|
Expiratory Disproportion Index (EDI) |
>50 |
>50 |
>50 |
|
FEV1/FEV0.5 Ratio |
≥1.5 |
≥1.5 |
≥1.5 |
FEV1=forced expiratory volume in one second; FEV0.5= forced expiratory volume in 0.5 second; FEF=forced expiratory flows; PEF=Peak Expiratory Flow; FIF50%= mid-inspiratory flow measured at 50% of the Forced Vital Capacity
SPECIFIC IMPORTANT APPLICATIONS OF PULMONARY FUNCTION TESTS
Upper airway obstruction versus Chronic obstructive pulmonary disease (COPD)
Usually, expiratory flow rate is affected both in upper airway obstruction as well as COPD and emphysema. There fore ,the shape of FVL alone would beinsufficient for precise diagnosis. Instead, four parameters need to be assessed simultaneously to suggest upper airway obstruction rather than COPD: FEV1/PEFR ≥10 ml/L/min, FIF50% ≤100 L/min, FEF50%/FIF50% ≥1, and FEV1/FEV0.5 ≥1.5.12,13
Paradoxical vocal fold movement disorder(PVFMD)&subglottic stenosis in non-obese
Paradoxical vocal fold movement disorder (PVFMD) and subglottic stenosis (SGS) are examples of extrathoracic airway obstruction and usually have similar symptoms. Flexible laryngoscopy sometimes cannot examine the subglottis completely. Therefore, PFT parameters, and EDI in particular, can be used to differentiate between these similar disorders. PEFR and FEV1/PEFR or EDI are significantly different in these disorders,15 and whether the patients are obese or not will generate a different EDI.16
Paradoxical vocal fold movement disorder (PVFMD)&subglottic stenosis (SGS) in obese
EDI is used to differentiate between PVFMD and SGS in all types of patients regardless of their BMI. However, EDI is a more sensitive parameter in non-obese patients and less sensitive in obese patients. One study found that the mean EDI in non-obese SGS was 69.32 and 48.38 in PVFMD patients. In obese patients, the mean EDI of SGS was 58.89 and 47.67 in obese PVFMD patients.16 Another study found that the mean EDI was 66.53 in non-obese stenotic and 49.55 in non-stenotic patients, while the mean EDI was 58.00 and 45.02 in the obese stenotic and non-stenotic patients, respectively.15 Therefore, EDI should be used carefully in obese patients and should not be a key marker in the diagnosis of such patients.16
Assessment of surgical intervention in tracheal stenosis
Tracheal stenosis, which is a decrease in the tracheal diameter distal to the cricoid cartilage, is diagnosed by several tools including laryngobronchoscopy. Spirometry can be a very helpful noninvasive diagnostic tool, especially Peak Expiratory Flow (PEF), to assess and predict surgical intervention in tracheal stenosis pre and post operatively.17 In addition, FEV1, FEF25%, FEF50%, MMEF and EDI are other parameters that could be good assessment tools while FVC and FEF75% are not the appropriate parameters to be used in such a situation.17
Assessment of surgical dilatation of subglottic stenosis
As a routine evaluation of subglottic stenosis, endoscopic assessment as well as clinical examinations are being used for the diagnosis of subglottic stenosis. Parameters such as PEF, FEV1, FEV1/PEF, FEF25, FEF50, FEF75, and MMEF are very useful prognostic values for surgical intervention and post-operative outcome.18
Role of spirometry in thoracic surgeries
Assessing whether the patient is a good candidate for thoracic surgery or not is of great value before taking the risk to jeopardize the patient's life. In addition, pulmonary function tests can be used to evaluate the outcome of thoracic surgery, especially FEV1. If FEV1 is less than 40% preoperatively, the lung resection is contraindicated while if FEV1 is more than 40%, the patient can go for pneumonectomy. Some researchers specified that FEV1 should be>60% for patient to undergo pneumonectomy or lobectomy.19-21
Role of spirometry in non-thoracic surgeries
The impact of respiratory complications, especially with high risk factor patients such as smokers, has to be considered when the patient is undergoing surgical procedure. Spirometry occasionally is not routinely indicated in non-thoracic surgeries. Pre-operative evaluation using pulmonary function tests is advocated to assess the risk of postoperative pulmonary complications. In patients with COPD, FEV1/FVC less than 50%, maximum voluntary ventilation 50%, or a high PaCO2 place the patient at a higher risk for postoperative complications. FEV1 or DLCO values <20% of predicted were associated with an unacceptably high postoperative mortality.19,22
Role of spirometry in predicting hospitalization and mortality in COPD
The prognosis of chronic obstructive pulmonary disease has huge concern to health organizations as well as to governments. BODE (Body mass index, airflow Obstruction, Dyspnea, and Exercise capacity) index which consists of body mass index, obstruction, dyspnea, exercise tolerance has been advocated to evaluate the prognosis of COPD patients with grading system. FEV1 parameter, as Part of BODE index, shows the importance of pulmonary function tests and hence more attention has to be directed toward their role.23
Flow volume loop in unilateral bronchial stenosis
Several pathological conditions such as granulationtissues, especially post lung transplantation, bronchomalacia, sarcoidosis, relapsing polychondritis, and bronchial carcinoma can lead to unilateral obstruction. Health care provider has to be very careful in diagnosing these cases. In such cases, the importance of flow volume curve will be certainly present. Occasionally, pulmonary function tests show obstructive pattern (significant decrease in FEV1 in addition to decrease FVC). The shape of flow volume loop also shows “biphasic flow volume loop” or “two can effect” due to slow emptying and filling of the affected lung (Figure 1). One lung usually fills/empty normally which gives normal curve while the other fills slowly due to the unilateral obstruction which gives the other phase of curve.24
Obstructive sleep apnea
Obstructive sleep apnea (OSA) is known to cause intermittent nocturnal hypopharyngeal obstruction and is considered as an upper airway obstruction. Even though the gold standard measure to detect sleep apnea is Apnea-Hypopnea Index (AHI) or critical closing pressure (Pcrit), flow-volume loop can be helpful. The flow-volume loop has a saw tooth sign (regular oscillations in forced expiratory or inspiratory FVL). This characteristic can also be seen in Parkinson’s disease and episodic laryngeal dyskinesia. Therefore, other diagnostic tools must be used to differentiate between these disorders.25 Table II shows summary of utility of Spirometry in special clinical situations.
Table II: SUMMARY OF UTILITY OF SPIROMETRY IN SPECIAL CLINICAL SITUATIONS
|
|
Clinical situations |
Important features |
|
1 |
Upper airway obstruction versus COPD |
FEV1/PEFR ≥ 10 ml/L/min FIF50% ≤ 100 L/min FEF50%/FIF50% ≥ 1 FEV1/FEV0.5 ≥ 1.5 |
|
2 |
Paradoxical vocal fold movement disorder (PVFMD) & subglottic stenosis in non-obese |
EDI=66-70 in non-obese EDI=45-50 in PVFMD |
|
3 |
Paradoxical vocal fold movement disorder (PVFMD) & subglottic stenosis in obese |
EDI= 58 in obese EDI= 45-50 in PVFMD |
|
4 |
Assessment of surgical intervention in tracheal stenosis |
PEF, FEV1, FEF25%, FEF50%, MMEF, EDI |
|
5 |
Assessment of surgical dilatation of subglottic stenosis |
PEF, FEV1, FEV1/PEF, FEF25, FEF50, FEF75, and MMEF |
|
6 |
Role of spirometry in thoracic surgery |
If FEV1 <40% preoperatively, lung resection is contraindicated while if FEV1 >40%, patient can go for pneumonectomy. FEV1 should be >60% for patient to undergo pneumonectomy or lobectomy |
|
7 |
Role of spirometry in non-thoracic surgeries |
With COPD, FEVI/FVC < 50%, MVV 50%, or high PaCO2, patients are at a higher risk for postoperative complications. FEV1 or DLCO values < 20% of predicted were associated with an unacceptably high postoperative mortality |
|
8 |
Role of spirometry in predicting hospitalization and mortality in COPD |
BODE (FEV1 is part of the mentioned index) |
|
9 |
Unilateral bronchial stenosis |
The shape of flow volume loop shows biphasic flow volume loop or two can affect. |
|
10 |
Obstructive sleep apnea |
Sawtooth sign (regular oscillations in forced expiratory or inspiratory FVL) |
COPD=Chronic Obstructive Pulmonary Disease; FEV1=forced expiratory volume in one second; FEV0.5= forced expiratory volume in 0.5 second; FEF=forced expiratory flows; PEF=Peak Expiratory Flow; FIF50%= mid-inspiratory flow measured at 50% of the FVC; DLCO: diffusing capacity of the lungs for carbon monoxide
CONCLUSION AND RECOMMENDATIONS
Various physiological lung parameters should be examined simultaneously to determine the precise diagnosis of upper airway obstruction. Relying on Spirometrical parameters alone or FVL alone and neglecting others might lead to misdiagnosis and subsequent mismanagement.
The shape of the FVL changes earlier than spirometrical parameters. The shape of the FVL, the Forced Expiratory Flow at 50% of vital capacity/Forced Inspiratory Flow at 50% of vital capacity (FEF-50%/FIF-50%) ratio, FEV1/FEV0.5, and the Empey index, along with the revised version of the EDI are of great value in diagnosing different types of upper airway obstructions.
Medical interns and residents should have thorough knowledge and understanding about these tools and their significance in order to apply them in their clinical practice.
REFERENCES
1. Brusasco V, Pellegrino R. Pulmonary function interpretative strategies: from statistics to clinical practice. Eur Respir J 2022;60(1):2200317. https://doi.org/10.1183/13993003.00317-2022
2. Gautam G, Michael Lippmann M. Disorders of the Central Airways and Upper Airway Obstruction. Pulmonary Medicine.Accessed on: June 10, 2022. Available from URL: https://www.pulmonologyadvisor.com/home/decision-support-in-medicine/pulmonary-medicine/disorders-of-the-central-airways-and-upper-airway-obstruction/
3. Sarkar M, Madabhavi IV, Mehta S, Mohanty S. Use of flow volume curve to evaluate large airway obstruction. Monaldi Arch Chest Dis 2022;92(4). https://doi.org/10.4081/monaldi.2022.1947
4. Won C, Michaud G, Kryger MH. Upper Airway Obstruction in Adults. In: Grippi MA, Elias JA, Fishman JA, Kotloff RM, Pack AI, Senior RM, Siegel MD. eds. Fishman's Pulmonary Diseases and Disorders, Fifth Edition. McGraw Hill; 2015. Accessed on: June 02, 2022. Available from URL: https://accessmedicine.mhmedical.com/content.aspx?bookid=1344§ionid=81189315
5. Sanchez-Guerrero J, Guerlain J, Samaha S, Burgess A, Lacau St Guily J, Périé S. Upper airway obstruction assessment: Peak inspiratory flow and clinical COPD Questionnaire. Clin Otolaryngol 2018;43(5):1303-11. http://doi.org/10.1111/coa.13149
6. Aboussouan L, Stoller J. Diagnosis and management of upper airway obstruction. Clin Chest Med 1994;15(1):35-53.
7. Karkhanis V, Desai U, Joshi J. Flow volume loop as a diagnostic marker. Lung India 2013;30(2):166-8. https://doi.org/10.4103/0970-2113.110435
8. Nouraei S, Franco R, Dowdall J, Nouraei S, Mills H, Virk J, et al. Physiology-based minimum clinically important difference thresholds in adult laryngotracheal stenosis. Laryngoscope 2014;124(10):2313-20. https://doi.org/10.1002/lary.24641
9. Carpenter D, Ferrante S, Bakos S, Clary M, Gelbard A, Daniero J. Utility of routine spirometry measures for surveillance of idiopathic subglottic stenosis. JAMA Otolaryngol Head Neck Surg 2019;145(1):21-6. https://doi.org/10.1001/jamaoto.2018.2717
10. Fiorelli A, Poggi C, Ardò NP, Messina G, Andreetti C, Venuta F, et al. Flow-volume curve analysis for predicting recurrence after endoscopic dilation of airway stenosis. Ann Thorac Surg 2019;108(1):203-10. https://doi.org/10.1016/j.athoracsur.2019.01.075
11. Al-Khlaiwi T. Flow volume curve: A diagnostic tool in extrathoracic airway obstruction. Pak J Med Sci 2020;36(4):846-7. https://doi.org/10.12669/pjms.36.4.2283
12. Empey DW. Assessment of upper airways obstruction. BMJ 1972;3(5825):503-5.https://doi.org/10.1136/bmj.3.5825.503
13. Rotman H, Liss H, Weg J. Diagnosis of upper airway obstruction by pulmonary function testing. Chest 1975;68(6):796-9. https://doi.org/10.1378/chest.68.6.796
14. Nouraei S, Nouraei S, Patel A, Murphy K, Giussani D, Koury E, et al. Diagnosis of laryngotracheal stenosis from routine pulmonary physiology using the expiratory disproportion index. Laryngoscope 2013;123(12):3099-104. https://doi.org/10.1002/lary.24192
15. Soldatova L, Hrelec C, Matrka L. Can PFTS differentiate PVFMD from subglottic stenosis? Ann Otol Rhinol Laryngol 2016;125(12):959-64. https://doi.org/10.1177/0003489416665195
16. Calamari K, Politano S, Matrka L. Can the Expiratory Disproportion Index distinguish PVFMD from subglottic stenosis in obese patients? Ann Otol Rhinol Laryngol 2021;1:3489421990154. https://doi.org/10.1177/0003489421990154
17. Alrabiah A, Almohanna S, Aljasser A, Zakzouk A, Habib S, Almohizea M, et al. Utility of spirometry values for evaluating tracheal stenosis patients before and after balloon dilation. Ear Nose Throat J 2020:145561320936968. https://doi.org/10.1177/0145561320936968
18. Abdullah A, Alrabiah A, Habib S, Aljathlany Y, Aljasser A, Bukhari M, et al. The value of spirometry in subglottic stenosis. Ear Nose Throat J 2019;98(2):98-101. https://doi.org/10.1177/0145561318823309
19. Mares-Gutiérrez Y, Salinas-Escudero G, Aracena-Genao B, Martínez-González A, García-Minjares M, Flores YN. Preoperative risk assessment and spirometry is a cost-effective strategy to reduce post-operative complications and mortality in Mexico. PLoS One 2022;17(7):e0271953. https://doi.org/10.1371/journal.pone.0271953
20. Brunelli A, Kim A, Berger K, Addrizzo-Harris D. Physiologic evaluation of the patient with lung cancer being considered for resectional surgery: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143(5 Suppl):e166S-e190S. https://doi.org/10.1378/chest.12-2395. Erratum in: Chest. 2014 Feb;145(2):437.
21. Shell D. Improving survival after pulmonary metastasectomy for sarcoma: analysis of prognostic factors. Gen Thorac Cardiovasc Surg 2023 Jan 12. https://doi.org/10.1007/s11748-023-01905-y
22. Grigorakos L, Sotiriou E, Koulendi D, Michail A, Alevizou S, Evagelopoulou P, et al. Preoperative pulmonary evaluation (PPE) as a prognostic factor in patients undergoing upper abdominal surgery. Hepatogastroenterology 2008;55(85):1229-32.
23. Vieira E, Degani-Costa L, Amorim B, Oliveira L, Miranda-Silva T, Sperandio PC, et al. Modified BODE Index to predict mortality in individuals with COPD: The Role of 4-Min Step Test. Respir Care 2020;65(7):977-83. https://doi.org/10.4187/respcare.06991
24. Agrawal A, Sahni S, Marder G, Shah R, Talwar A. Biphasic flow-volume loop in granulomatosis with polyangiitis related unilateral bronchus obstruction.Respiratory Investigation2016;(54)4:280-83. https://doi.org/10.1016/j.resinv.2016.01.002
25. Slowik JM, Sankari A, Collen JF. Obstructive Sleep Apnea. 2022 Jun 28. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan. Accessed on: June 10, 2022. Available from URL: https://www.ncbi.nlm.nih.gov/books/NBK459252/
|
Following authors have made substantial contributions to the manuscript as under:
TAl-K & SSH: Concept and study design, acquisition, analysis and interpretation of data, drafting the manuscript, critical review, approval of the final version to be published.
Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |