![]() https://doi.org/10.35845/kmuj.2023.22983 ORIGINAL
ARTICLE
https://doi.org/10.35845/kmuj.2023.22983 ORIGINAL
ARTICLE
Impact of socio-economic status on Diabetes Mellitus knowledge and hemoglobin A1c control
Malick
Maria Alvi1![]() ,
Sumerah Jabeen1, Faisal Zahid1, Ayesha Jabeen 1,
Ahmed Raheem Buksh1
,
Sumerah Jabeen1, Faisal Zahid1, Ayesha Jabeen 1,
Ahmed Raheem Buksh1
|
1: Patel Hospital, Karachi, Pakistan
Email Contact #: +92-336-3230240 Date Submitted: February 07, 2022 Date Revised: April09, 2023 Date Accepted: August 21, 2023 |
|
THIS ARTICLE MAY BE CITED AS:Alvi MM, Jabeen S, Zahid F, Buksh AR, Jabeen A. Impact of socio-economic status on diabetes mellitus knowledge and hemoglobin A1c control. Khyber Med Univ J 2023;15(3):176-82. https://doi.org/10.35845/kmuj.2023.22983 |
ABSTRACT
OBJECTIVE: To assess the impact of socioeconomic status (SES) on Diabetes Mellitus (DM) knowledge and glycemic control among diabetic patients in Pakistan, considering the rising prevalence of DM and its associated economic burden.
METHODS: This cross-sectional study was conducted over three months at a tertiary care hospital in 2020, involving 235 DM patients aged 20 to 75 years. The Diabetes Knowledge Questionnaire (DKQ) and modified Kuppuswamy index were employed to evaluate diabetes knowledge and SES, respectively. Glycemic control was assessed using hemoglobin A1c (HbA1c) levels, and statistical analyses were performed.
RESULTS: Among 230 analyzed participants, 121 (52.4%) were females and 109 (47%) were males. Majority were type-2 DM (n=207; 90%). Mean age was 57.1±13.61 years, mean duration of DM was 14.07±9.54 years and mean Body Mass Index was 29.64±6.1 kg/m2. Majority of participants were from the upper-middle (n=93; 40.4%) and lower-middle class (n=93; 40.4%); 20 (8.7%) were from lower class and 24 (10.4%) from upper class. The study revealed a strong impact of SES on diabetes knowledge (p=0.000*), with a gradual improvement from lower to upper classes. Similarly, SES significantly influenced glycemic control (p=0.005*), demonstrating a pattern of increased knowledge and improved glycemic control with higher socioeconomic status.
CONCLUSION: This study underscores the significant relationship between socioeconomic status, diabetes knowledge, and glycemic control among Pakistani diabetic patients. Improved disease knowledge and better glycemic control were associated with higher socioeconomic classes, emphasizing the need for tailored educational interventions and healthcare strategies to mitigate the impact of diabetes in diverse socioeconomic groups.
KEYWORDS: Diabetes Mellitus (MeSH); Diabetes Knowledge (Non-MeSH); Social Class (MeSH); Pakistan (MeSH);Glycated Hemoglobin (MeSH).
INTRODUCTION
There are 573 million people living with diabetes worldwide making it a disease of 1 in every 10 individuals.1It imposes a great challenge to the health authorities as growing urbanization, sedentary lifestyle with massive surge in obesity are all contributing factors to this “diabetes epidemic”.
Recent years have shown a rapid rise of diabetes among South Asian population, which inflicts a significant health concern with more aggressive progression compared to other ethnic groups.2,3As per International Diabetes federation figures,in Pakistan there are 33 million adults living with diabetes which is a 70% rise in prevalence since 2019,ranking Pakistan 3rd in the world for having the highest number of diabetic patients1. This high prevalence of diabetes among countries is a source of significant economic burden, rising medical expenditures, and treatment of complications.4,5Studies have shown that improved diabetes knowledge is related to better glycemic control, disease outcomes, and prevention of diabetes complications.6,7
The disease knowledge can be pivotal in achieving the targeted outcomes by utilizing the gaps in knowledge. It can further assist in formulating innovative tools, educational models and health education programs leading to better compliance and practices among diabetic patients.7 On the contrary, in lower socioeconomic populations because of lack of provision of health facilities and education, insufficient diabetes knowledge and its related complication prevail.8,9
Multiple studies have been conducted in Pakistan documenting the diabetes knowledge in general population and diabetic patients but according to our knowledge there has been no study to date which has determined the impact of socioeconomic status (SES) on diabetes knowledge and glycemic control among diabetic patients.
This study would be helpful to determine if an association exists between better SES leading to improved diabetes awareness and disease outcome i.e.hemoglobin A1c (HbA1c) levels in a developing country like Pakistan. This knowledge can have far-reaching implications on how a stable economy can lead to a healthier population, reducing disease burden, and improving quality of life. Also, the need for designing educational programs and interventions as per the socioeconomic classes for better diabetes knowledge and practice.
METHODS
After Internal Board Review approval, this is a cross-sectional study which was conducted at our institute during a period of three months from June 2020 to September 2020. The total study participants were 235 which was calculated using the Open Epi program (version 3), by keeping a two-sided bconfidence interval of 95%. All the patients diagnosed as diabetes mellitus type 1 and type2, on insulin therapy or oral hypoglycemic, with age limit between 20 to 75 years of age with or without complication of diabetes mellitus with any economic status were included in the study. Mentally challenged, psychiatric patients and dementia patients, Unconscious patients excluded from the study and patients with communication / language barrier were excluded from the study.
All diabetic patients who had either one or two visits to the medical and diabetic OPD of Patel hospital or those who got admitted with diabetic complications were incorporated in the study after getting written informed consent. Data was collected by consecutive purposive sampling. Study participants were assessed for knowledge regarding diabetes mellitus. The socioeconomic status was evaluated by a predefined questionnaire, including details of demography, Diabetes knowledge test questions, questions related to education, profession and household income of individual. Questionnaire in Urdu language was also provided. Diabetes knowledge was assessed by using the Diabetes Knowledge Questionnaire (DKQ). It is a 24-item questionnaire, designed by Starr County Diabetes Education Study, to get the information about patients' understanding of the cause, complications and symptoms as well as treatment of disease. Glycemic control was assessed by HbA1C taken within 3 months, less than 7.5% was taken to be statistically significant glycemic control. Socio-economic status was assessed by modified Kuppuswamy index 2019. For illiterate participants, questions were explained to participants, by the investigators.
Diabetes knowledge: Diabetes Knowledge in this study has been described as the understanding of information regarding diabetes on 24 items which is given in the questionnaire. The Diabetes Knowledge Questionnaire(DKQ) comprises of 24-item questionnaire, which is designed by Starr County Diabetes Education Study, to get the information of patient’s knowledge regarding understanding of etiology of disease, its related complications, importance of physical activity, target blood glucose levels, and also knowledge of diabetic diet. This DKQ has been translated into the local language of Pakistan, Urdu and validated.10 It has three response options for each question "yes", "no", and "don't know”. One point is given for each correct option, whereas, no point for the incorrect option. By summing up the points the total score is estimated for each patient. A higher score represents better disease knowledge. In this study score of less than 10 was regarded as poor knowledge. The score between 11 and 17 taken as average knowledge and more than 17 was taken as good knowledge.
Kappuswammy score: This is a composite score of socioeconomic scale which is used to measure socioeconomic status in urban and rural areas. It includes education of the head of family, its occupation as well as the monthly income of family. It divides the socioeconomic status in to five classes namely, upper class, upper middle class, lower middle class, upper lower class, and lower class with scores from 1 to 29. Lower class scores 1 to 4, upper lower-class scores 5 to 10, lower middle-class scores 11 to 15 and upper middle-class scores 16 to 25-, and upper-class scores 26 to 29.
Most of the public health and medical research include economic and social status as one of the pertinent predictors for health-related variables at the individual or family level. This score is originated from India. Because of its comprehensive scoring technique, we included this score in our research as Pakistan is also a developing country of Southeast Asia with similar socioeconomic challenges as in India. Only monthly income of heads of family is modified according to the Pakistani income.
Education of head of family was divided into professional degree, graduate or postgraduate degree, intermediate school, education till high school, middle school education, primary school education or illiterate, all parts were given specific scores accordingly, similarly profession of head of family comprised of different parts namely professional, semiprofessional, clerical, skilled worker, unskilled worker and unemployed, likely all parts were given separate scores. Monthly income of head of family was modified according to the Pakistani currency. It was divided into different income ranges. Monthly household income taken in Rupees, less than 15000 were given scores of 1, 16,000 to 30,000 were given score of2, 31,000 to 50,000 scored as 3, 51,000 to 70,000 scored 4,71,000 to 100,000 score of 6,100,001 to 150,000 score of 10 and more than 150,000 score of 12. These three factors scores were combined to set a socioeconomic status of a person.
Socioeconomic status: According to American Psychological Association, socioeconomic status is described as the social status, rank or position of an individual or group. It is often measured as a blend of education, monthly income, and occupation. For assessment of socioeconomic status modified Kuppuswamy scale was used and adjusted according to Pakistani currency.11
Statistical analysis: SPSS version 22 was used for the analysis of participant’s data. Data was stratified quantitatively and descriptively. Quantitative variables (such as age, duration of diabetes) were calculated by mean and standard deviation. Independent variables are age, gender, duration of diabetes and socioeconomic status, while dependent variables are diabetes knowledge and HbA1c levels. Qualitative variables (gender, socioeconomic status, educationor treatment taken for diabetes and glycemic control) were depicted as frequencies and percentages. SES, glycemic control are qualitative variables as they are shown in categories so they are ordinal qualititative variables. For the estimation of association of SES with diabetes knowledge, andHbA1c levels chi –square test was used. Association of diabetes knowledge with age and duration of diabetes Anova test was used. P-value of < 0.05 has been taken as statistically significant.
RESULTS
In our study, 235 diabetic patients were enquired about their knowledge of diabetes and their socioeconomic status by a pre-specified questionnaire. For assessing diabetes knowledge DKQ questionnaire was used and for assessingthe socioeconomic status of the patient Kuppuswamy score was used which was modified according to the value of Pakistani currency. Data of 5 participants were not included due to incomplete information. HbA1C levels within 3 months’ duration were also recorded.Two hundred and thirty participants were analyzed. In our study mean age of participants was 57.1 years (±13.61), 52.4%[n=121] were female, and 47%[n=109] were male. The calculatedmean duration of diabetes mellitus was 14.07±9.54yearswith a range (2 months to 40 years), the mean BMI of the patients was 29.64 with a range of (16.6 to 47.84). Most of the participants [90% (n=207)] were type-2 diabetic while 10%[n=23] were type-1 diabetics. Half of the patients (50%) had a family history of diabetes in the close relatives while 10% of participants had no family history of diabetes. Moreover, 23% had a positive family history of diabetes mellitus in both first and second-degree relatives. Demographic characteristics of the participantsare shown in Table I.
Table I: Demographic characteristics of the study participants
|
Descriptive Statistics |
Mean ± SD |
Range (Min – Max) |
|
Age (years) |
57.14 (±13.61) |
(21 - 85) |
|
Duration of Diabetes Mellitus(years) |
14.07 (±9.54) |
(0.15 - 40) |
|
Body Mass Index (kg/m2) |
29.64 (±6.1) |
(16.6 - 47.84) |
|
Education score |
4.55 (±1.68) |
(1 - 7) |
|
Occupation Score |
5.89 (±2.36) |
(1 - 10) |
|
Monthly Income Score |
6.03 (±2.81) |
(2 - 12) |
In our study, participants from the middle class were found to be in the highest percentage 40.4%[n=93] from upper middle class and 40.4%[n=93] from lower middle class. The majority 39%[n=90] of participants had a graduate degree while only 2.6%[n=6] were illiterate,25.7%[n=59] were semi-professionals followed by skilled workers 23.9%[n=55] and professionals 21.1%[n=49]. Majorityof participants 33%[n=76] had the monthly household income of 51000 to 70000 rupees followed by 30%[n=70] of participants with a monthly income of 70,000 to 1 lac rupees. Percentage of correct answer of different diabetes knowledge question is shown in Table II.
Table II: Percentage of correct answer of diabetes knowledge questionnaire
|
Diabetes Knowledge Questionnaire for assessing diabetes knowledge (n=230) |
Correct |
|
|
1 |
Eating too much sugar and other sweet foods is a cause of diabetes. |
31.7% |
|
2 |
The usual cause of diabetes is lack of effective insulin in the body. |
49.6% |
|
3 |
Diabetes is caused by failure of the kidneys to keep sugar out of the urine. |
25.2% |
|
4 |
Kidneys produce insulin |
0.0% |
|
5 |
In untreated diabetes, the amount of sugar in the blood usually increases. |
92.6% |
|
6 |
If I am diabetic, my children have a higher chance of being diabetic. |
60.4% |
|
7 |
Diabetes can be cured |
37.0% |
|
8 |
A fasting blood sugar level of 210 is too high. |
73.5% |
|
9 |
The best way to check my diabetes is by testing my urine |
45.2% |
|
10 |
Regular exercise will increase the need for insulin or other diabetic medication. |
54.3% |
|
11 |
There are two main types of diabetes: Type 1 (insulin-dependent) and Type 2 (non-insulin-dependent). |
33.0% |
|
12 |
An insulin reaction is caused by too much food. |
28.7% |
|
13 |
Medication is more important than diet and exercise to control my diabetes. |
58.7% |
|
14 |
Diabetes often causes poor circulation |
51.3% |
|
15 |
Cuts and abrasions on diabetics heal more slowly |
90.0% |
|
16 |
Diabetics should take extra care when cutting their toenails. |
65.2% |
|
17 |
A person with diabetes should cleanse a cut with iodine and alcohol. |
19.6% |
|
18 |
The way I prepare my food is as important as the foods I eat. |
32.2% |
|
19 |
Diabetes can damage my kidneys. |
71.7% |
|
20 |
Diabetes can cause loss of feeling in my hands, fingers, and feet |
73.5% |
|
21 |
Shaking and sweating are signs of high blood sugar. |
0.0% |
|
22 |
Frequent urination and thirst are signs of low blood sugar |
46.5% |
|
23 |
Tight elastic hose or socks are not bad for diabetics. |
31.3% |
|
24 |
A diabetic diet consists mostly of special foods. |
33.5% |
Table III shows Strong impact of socioeconomic status [SES] of diabetic patients on diabetes knowledge, suggesting a significant relationship between them with a p-value of 0.000* by applying chi-square test. It was found that among the lower class,90%[n=18] had poor knowledge(from upper lower socioeconomic class) and only 10% had average knowledge. Among middle class participants, the knowledge improved gradually as the interclass status ascended, 37.8% [n=48] had average knowledge from lower middle class which was improved to 45.7% [n=58] in the upper middle-class. It was found that upper class had the highest ratio of disease knowledge i.e., from overall 24participants from this class 74% [n=19] had average knowledge and only 20%(n=5) had poor knowledge. Duration of diabetes was not having significant impact on knowledge of participants (p-value 0.799), Age of participants were not associated with good knowledge of diabetes (p-value=0.179).
Similarly, significant impact of socioeconomic status was observed on HbA1C levels of diabetic patientswith p-value of 0.005* by applying chi-square test. Only25% [n=5] patients from lower class had good glycemic control (HbA1c of less than 7.5%)while 75% of patients from this class had uncontrolled HbA1C levels, similarly 34%[n=32] and 55% [n=52] of participants showed good glycemic control from lower middle and upper middle class respectively, while 66% [n=16] of participants from upper class showed improved glycemic control. So, this indicates a gradual pattern of increase in knowledge and improved glycemic control as the socioeconomic status improves.
Table III: Comparison of diabetic knowledge among different demographics, clinical, socioeconomic class, and HbA1c level
|
Demographics & |
Diabetes Knowledge |
p-value
|
|||
|
Poor [n=99] |
Average [n=127] |
Good Knowledge [n=4] |
|||
|
Age in (years) |
58.9 ± 12.6 |
56 ± 14.4 |
50.5 ± 7.5 |
0.175 |
|
|
Duration of Diabetes Mellitus (in years) |
14.6 ± 8.8 |
13.7 ± 10.1 |
13.8 ± 11 |
0.799 |
|
|
Body mass index (BMI) kg/m2 |
30.3 ± 5.9 |
29 ± 6.2 |
31.7 ± 8.3 |
0.21 |
|
|
Gender of patients |
Male |
49 (49.5%) |
59 (46.5%) |
1 (25%) |
0.599 |
|
Female |
50 (50.5%) |
68 (53.5%) |
3 (75%) |
||
|
Type of diabetes |
Type 1 diabetes |
6 (6.1%) |
17 (13.4%) |
0 (0%) |
0.152 |
|
Type 2 diabetes |
93 (93.9%) |
110 (86.6%) |
4 (100%) |
||
|
HbA1c levels checked within 3 months period |
Less than 7.5% |
27 (27.3%) |
78 (61.4%) |
0 (0%) |
0.000* |
|
7.6% to 8.9% |
36 (36.4%) |
33 (26%) |
2 (50%) |
||
|
9% and more than 9% |
36 (36.4%) |
16 (12.6%) |
2 (50%) |
||
|
Total |
99 (100%) |
127 (100%) |
4 (100%) |
|
|
|
Socioeconomic class |
Upper class |
5 (5.1%) |
19 (15%) |
0 (0%) |
0.000* |
|
Upper middle class |
34 (34.3%) |
58 (45.7%) |
1 (25%) |
||
|
Lower middle class |
42 (42.4%) |
48 (37.8%) |
3 (75%) |
||
|
Upper lower class |
18 (18.2%) |
2 (1.6%) |
0 (0%) |
||
|
Lower class |
0 (0%) |
0 (0%) |
0 (0%) |
||
|
Education of head of family |
Not educated / illiterate |
5 (5.1%) |
1 (0.8%) |
0 (0%) |
0.025* |
|
Primary level education |
19 (19.2%) |
7 (5.5%) |
0 (0%) |
||
|
Secondary level education |
19 (19.2%) |
18 (14.2%) |
1 (25%) |
||
|
High school education |
21 (21.2%) |
30 (23.6%) |
1 (25%) |
||
|
Graduate degree |
30 (30.3%) |
58 (45.7%) |
2 (50%) |
||
|
Professional degree |
5 (5.1%) |
13 (10.2%) |
0 (0%) |
||
Fisher exact/Chi-square, Parametric anova test was applied. at 95% Confidence interval (C.I),
Table IV shows comparison of SES with HbA1c levels.
Our study showed that knowledge of diabetes etiology, diabetes inheritance, correct fasting blood sugars and impact of exercise on the improving diabetes control was significantly related to the socioeconomic status of patients.
|
Socioeconomic class |
HbA1c levels checked within 3 months period |
Total |
p-value# |
||
|
Less Than 7.5% |
7.6% to 8.9% |
More Than 9% |
|||
|
Upper Class |
16 |
4 |
4 |
24 |
0.005* |
|
Upper Middle Class |
52 |
22 |
19 |
93 |
|
|
Lower Middle Class |
32 |
38 |
23 |
93 |
|
|
Upper Lower Class |
5 |
7 |
8 |
20 |
|
|
Total |
105 |
71 |
54 |
230 |
|
# Chi-square test applied for estimating association between socio-economic status and HbA1c levels; HbA1C hemoglobin A1c
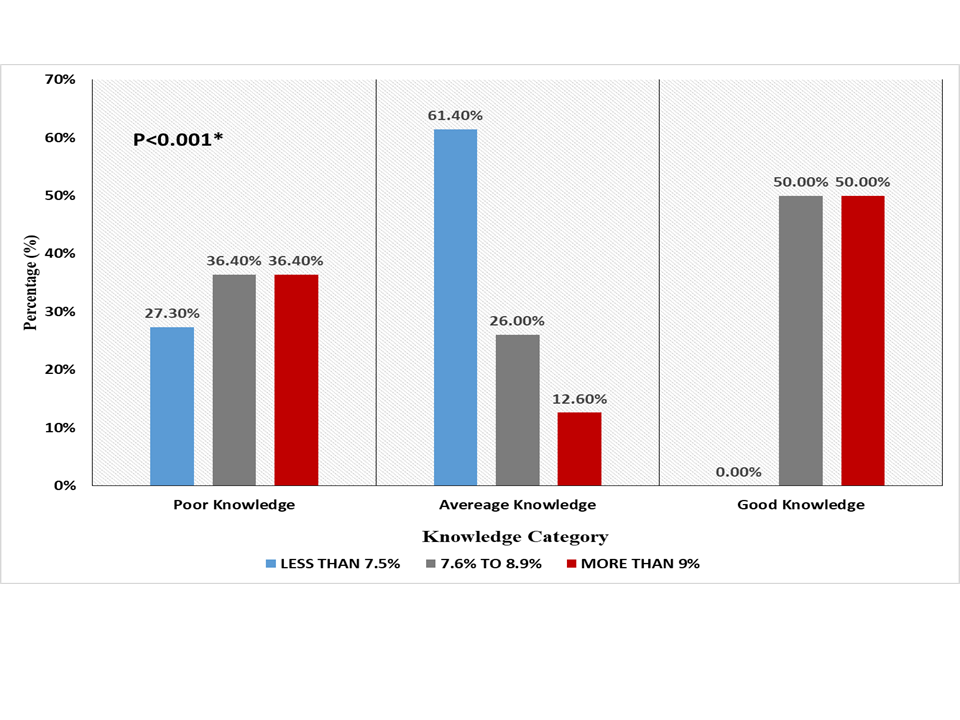
Association of diabetes knowledge score with HbA1c categories (<7.5%, 7.6% to 8.9% &>9%), checked within 3 months of duration is given in figure 1.
DISCUSSION
Diabetes Mellitus (DM) has reached epidemic levels around the world due to an alarming rise in numbers. In the last few decades, it has become an emerging health problem in developing countries.12 The objective of this study was to define the impact of socio-economic status on diabetes mellitus knowledge and HbA1c control.
Our data favors better diabetes control and diabetes knowledge with improving socioeconomic status.
This is the first study in Pakistan evaluating the impact of socioeconomic status on DM knowledge and diabetes control. The majority of participants included in the study were from the upper and lower middle class with the mean modified Kuppuswamy score of 16. Comparing the diabetes knowledge and glycemic control results among various socioeconomic classes, participants with higher incomes showed better diabetes awareness knowledge and HbA1C control compared to those with lower incomes. Our study findings resonate with data from other studies conducted in different countries. Cowie et al in describing the sociodemo graphic characteristics of patients with diabetes showed that people with lower SES had a greater prevalence of diabetes along with the increased burden of morbidity and mortality compared with people with better SES.13Among the various factors causing this co relation, depression has been proven to be a significant arbitrator in the relationship between SES and glycemic control. People living in poverty have been shown to interpret their futile efforts to control their diabetes as a sign of the unpredictable nature of the disease rather than the lack of efforts on their part.14There are also studies suggesting lower SES to higher stress levels which in turn can cause endocrine perturbations leading to type 2DM.15,16A study conducted by Tahirovic et al assessing the association between glycemic control in children with Type 1DM and socioeconomic status of the family showed lower SES was associated with higher HbA1c levels suggesting diabetes care has both direct and indirect costs.17 The EuroDiab IDDM complications study has also shown that men and women from lower SES classes had higher Hba1c levels.18
The socioeconomic impact on diabetes control in a developing country like Pakistan could be the result of the overall financial cost the disease carries with expenses ranging from medications to maintain glucose charts and frequent laboratory testing since diabetes care is not free in our country. Also people with better income have access to better diabetes care programs being run individually in bigger hospitals compared to those patients who due to financial constraints are deprived of basic medical facilities and diabetes education. Our study also showed that diabetes knowledge and control were better among participants with a graduate degree compared to those with secondary level education and below, implicating that education also has an impact on diabetes knowledge and control. Studies have validated that in diabetic population with ethnical diversity and low-income, literacy can partially bridge this gap , mediated by the practical relationship between good education and glycemic control.9 The demands of self-management in diabetes care can be a little overwhelming for an individual with inadequate literacy suggesting implications on education and health policy.19Individuals with inadequate literacy are shown to face problems with both the written and an oral form of communication in the clinical context.20
American Diabetes Association (ADA) recommends a comprehensive diabetes self-management education and support (DSMES) since it plays an important role in improving patient self-management, satisfaction, and glucose outcomes.21The majority of the participants in our study irrespective of class difference had good knowledge regarding target blood glucose levels and diabetes-related complications including neuropathy, nephropathy, and poor wound healing and proper nail cutting techniques. One probable reason for this widespread knowledge could be a high prevalence of such diabetes-related complications in our part of the world due to lack of proper follow-up system leading to delayed diagnosis and related complications. Although the above interpretation in our study is in alignment with the localstudy findings conducted by Shams et al where the majority of participants were well aware of diabetes complications but this contradicts with a study conducted in another province of Pakistan where most of the participants had poor knowledge regarding diabetes complications, pointing towards the additional demographic differences with bigger cities having more awareness compared to smaller cities of the country.22,23
Overall our study participants had poor knowledge regarding the pathophysiology and autonomic dysfunction related to hypo and hyperglycemia which could be interpreted as a limited transfer of knowledge between diabetes educators and the patients about the nature of the disease and its more prolonged complications, emphasizing the importance of a more comprehensive diabetes self-management and education programs among the general population and most important among patients with DM..
One of the limitations of our study is that most of the participants were from the middle class which could have affected the results. Also, our study participants were a limited number of diabetic patients attending outdoor clinics and inpatients at a tertiary care hospital therefore our findings might not be generalized to the diabetic population in Karachi/Pakistan and requires reinforcement through further work.
CONCLUSION
This research highlights the significant interplay among socioeconomic status, diabetes knowledge, and glycemic control within the Pakistani diabetic population. The study underscores the considerable influence of SES on disease awareness and HbA1c levels, accentuating the necessity for targeted educational interventions tailored to diverse socioeconomic classes. Higher socioeconomic status is linked to enhanced disease knowledge and improved glycemic control, reinforcing the importance of customized educational initiatives and healthcare strategies. Elevating socioeconomic status, coupled with accessible diabetes care programs, has the potential to enhance metabolic control, mitigate acute and chronic complications, and ultimately enhance overall quality of life.
REFERENCES
1. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes ResClin Pract 2022;183:109119.https://doi.org/10.1016/j.diabres.2021.109119
2. Mukhopadhyay B, Forouhi NG, Fisher BM, Kesson CM, Sattar N. A comparison of glycaemic and metabolic control over time among South Asian and European patients with type 2 diabetes: results from follow‐up in a routine diabetes clinic. Diabet Med 2006;23(1):94-8.https://doi.org/10.1111/j.1464-5491.2005.01735.x
3. Basit A, Fawwad A, Qureshi H, Shera AS, NDSP Members. Prevalence of diabetes, pre-diabetes and associated risk factors: second National Diabetes Survey of Pakistan (NDSP), 2016–2017. BMJ Open 2018;8(8):e020961.https://doi.org/10.1136/bmjopen-2017-020961
4. Karaoui LR, Deeb ME, Nasser L, Hallit S. Knowledge and practice of patients with diabetes mellitus in Lebanon: a cross-sectional study. BMC Public Health 2018;18(1):1-9.https://doi.org/10.1186/s12889-018-5416-7
6. Garcia AA, Villagomez ET, Brown SA, Kouzekanani K, Hanis CL. The Starr County Diabetes Education Study: development of the Spanish-language diabetes knowledge questionnaire. Diabetes Care 2001;24(1):16-21.https://doi.org/10.2337/diacare.24.1.16
7. Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther 2011;13(3):335-41.https://doi.org/10.1089/dia.2010.0160
8. Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep 2006;121(3):245-54.https://doi.org/10.1177/003335490612100305
9. Bukhsh A, Lee SWH, Pusparajah P, Khan AH, Khan TM. Psychometric properties of the Urdu version of diabetes knowledge questionnaire. Front Public Health 2017;5:139. https://doi.org/10.3389/fpubh.2017.00139
10. Wani RT. Socioeconomic status scales-modified Kuppuswamy and Udai Pareekh's scale updated for 2019. J Family Med Prim Care2019;8(6):1846-9.https://doi.org/10.4103/jfmpc.jfmpc_288_19
11. Jayawardena R, Ranasinghe P, Byrne NM, Soares MJ, Katulanda P, Hills AP. Prevalence and trends of the diabetes epidemic in South Asia: a systematic review and meta-analysis. BMC Public Health 2012;12(1):1-13.https://doi.org/10.1186/1471-2458-12-380
12. Menke A, Knowler WC, Cowie CC. Physical and Metabolic Characteristics of Persons With Diabetes and Prediabetes. In: Cowie CC, Casagrande SS, Menke A, et al., editors. Diabetes in America. 3rd edition. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases (US); 2018 Aug. CHAPTER 9. Accessed on: April 03, 2023. Available from URL: https://www.ncbi.nlm.nih.gov/books/NBK567973/
13. Houle J, Lauzier-Jobin F, Beaulieu MD, Meunier S, Coulombe S, Côté J, et al. Socioeconomic status and glycemic control in adult patients with type 2 diabetes: a mediation analysis. BMJ Open Diabetes Res Care 2016;4(1):e000184.https://doi.org/10.1136/bmjdrc-2015-000184
14. Meyer IH, Schwartz S, Frost DM. Social patterning of stress and coping: does disadvantaged social statuses confer more stress and fewer coping resources?. Social Sci Med 2008;67(3):368-79.https://doi.org/10.1016/j.socscimed.2008.03.012
15. Björntorp P, Holm G, Rosmond R. Hypothalamic arousal, insulin resistance and type 2 diabetes mellitus. Diabet Med 1999;16(5):373-83.https://doi.org/10.1046/j.1464-5491.1999.00067.x
16. Tahirovic H, Toromanovic A. Glycemic control in diabetic children: role of mother’s knowledge and socioeconomic status. Eur J Pediatr 2010;169(8):961-4.https://doi.org/10.1007/s00431-010-1156-0
17. Chaturvedi N, Stephenson JM, Fuller JH. The relationship between socioeconomic status and diabetes control and complications in the EURODIAB IDDM Complications Study. Diabetes Care 1996;19(5):423-30.https://doi.org/10.2337/diacare.19.5.423
18. Grant RW, Pirraglia PA, Meigs JB, Singer DE. Trends in complexity of diabetes care in the United States from 1991 to 2000. ArchIntern Med 2004;164(10):1134-9.https://doi.org/10.1001/archinte.164.10.1134
19. Schillinger D, Bindman A, Wang F, Stewart A, Piette J. Functional health literacy and the quality of physician–patient communication among diabetes patients. Patient Educ Couns 2004;52(3):315-23.https://doi.org/10.1016/s0738-3991(03)00107-1
20. American Diabetes Association. Glycemic targets: standards of medical care in diabetes—2019. Diabetes Care 2019;42(Suppl1):S61-70.https://doi.org/10.2337/dc19-s006
21. Shams N, Amjad S, Seetlani NK, Ahmed W. Diabetes knowledge in elderly type 2 diabetes mellitus patients and association with glycemic control. J Liaquat Uni Med Health Sci 2016;15(2):71-7.
22. Ullah F, Afridi AK, Rahim F, Ashfaq M, Khan S, Shabbier G, et al.Knowledge of diabetic complications in patients with diabetes mellitus. J Ayub Med Coll Abbottabad2015;27(2):360-3.
|
Following authors have made substantial contributions to the manuscript as under:
MMA& FZ: Conception, acquisition, analysis and interpretation of data, drafting the manuscript, approval of the final version to be published SJ: Study design, critical review, approval of the final version to be published AJ: Acquisition, analysis and interpretation of data, drafting the manuscript, approval of the final version to be published ARB: Analysis and interpretation of data, drafting the manuscript, approval of the final version to be published Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |