https://doi.org/10.35845/kmuj.2023.22928 CASEREPORT
https://doi.org/10.35845/kmuj.2023.22928 CASEREPORT
Restoration of subtotal bilateral maxillectomy defect following mucormycosis with zygomatic implant-retained obturator:a case report
Maria
ShakoorAbbasi1![]() ,
JehanAlam2
,
JehanAlam2
|
1: Department of Prosthodontics, Altamash Institute of Dental Medicine, Karachi, Pakistan 2: Dental Department, Jinnah Postgraduate Medical Center, Karachi, Pakistan
Email Contact #: +92-333-3615061 Date Submitted: June 29, 2022 Date Last Revised: April 03, 2023 Date Accepted: May 17, 2023 |
|
THIS ARTICLE MAY BE CITED AS:Abbasi MS, Alam J. Restoration of subtotal bilateral maxillectomy defect following mucormycosis with zygomatic implant-retained obturator: a case report. Khyber Med Univ J 2023;15(2):134-7. https://doi.org/10.35845/kmuj.2023.22928 |
ABSTRACT
INTRODUCTION: This clinical case report with a 5-year follow-up period describes the successful prosthetic rehabilitation of a patient who underwent subtotal bilateral maxillectomy for mucormycosis; a serious but rare fungal infection.
CASE PRESENTATION: A 65-year-old male presented with speech and eating difficulties post-maxillectomy due to mucormycosis. The consequential wide defect had involved the entire hard palate and most of the soft palate. A customized obturator, anchored by three zygomatic implants and one infraorbital rim implant, restored function and aesthetics. Precise implant placement and meticulous prosthetic design ensured optimal retention. Follow-ups showed sustained improvements in speech, chewing, and quality of life, with no complications.
CONCLUSION: Despite anatomic deficiencies, the patient's aesthetic and functional demands were fulfilled. Zygomatic implant-retained obturators offered an effective solution for maxillary defects, enhancing oral health and patient satisfaction.
KEYWORDS: Prosthetic rehabilitation (Non-MeSH); Subtotal bilateral maxillectomy (Non-MeSH); Zygomatic Implants (Non-MeSH).
INTRODUCTION
One of the most rewarding areas of prosthodontics is the rehabilitation of patients with the acquired maxillary defect. Maxilla is a very important structure in the midface, as it separates the oronasal and orbital cavities, provides support to their associated structures and plays a critical role in phonetics, deglutition, and mastication. Due to the partial or complete surgical resection of the maxilla, the patient develops unintelligible/ hypernasal speech, leakage of fluid into the nasal cavity and impaired masticatory functions due tooronasal communication.1,2Thus the greatest challenge lies in reestablishing this separation. For this purpose, a customized obturator prosthesis is generally used not only to close the palatal defect but also to restore the masticatory function and improve speech, deglutition and esthetics. An added advantage over autogenous tissue reconstruction is it simplifies oncological surveillance as well.3
The retention and stability of an obturator depend on the remaining dentition, the amount of residual bone and defect configuration. Sometimes, conventional obturator prosthesis is unable to provide adequate retention, stability and support. In such cases, precision attachments or implant-supported/ retained prostheseshave proven valuable.4 In addition, zygomatic implants have gained popularity over recent years for rehabilitation after tumor resection/trauma/atrophic maxilla without hard and soft tissue augmentations.5
This clinical case report describes the successful prosthetic rehabilitation of a patient who underwent subtotal bilateral maxillectomy for a serious but rare fungal infection called mucormycosis. The consequential wide defect that involved the entire hard palate and most of the soft palate was rehabilitated with an obturator prosthesis retained by three zygomatic implants and one infraorbital rim implant.
CASE REPORT
A 65-year-old male reported to Altamash Institute of Dental Medicine, Karachi, Pakistan on March, 2017 with a chief complaint of difficulty in eating and unintelligible speech. He further added that he was unable to sleep at night due to leakage and pooling of nasal secretion into the oral cavity. Past dental history revealed that he was diagnosed with a serious but rare fungal infection called mucormycosis, for which he underwent subtotal bilateral maxillectomy a year back. On extra-oral examination, the patient had a symmetric face with a straight profile and competent lips. The upper lip was thinned and fell back being devoid of the alveolar support from the maxilla. The temporomandibular joints were normal, with no pain, sounds, deviation or deflection on opening and closing. Maximum mouth opening was recorded up to 42mm. On intraoral examination, there was a large palatal defect that fell under class 2c according to Liverpool’s or browns classification of maxillary defects. Maxillary and mandibular impressions were recorded for the diagnostic casts. Extra and intra-oral photographs were taken. A digital orthopantomogram and cone beam computed tomography scan was advised. Treatment options were discussed with the patient and he opted for a zygomatic implant-retained maxillary obturator for replacing his dentition and associated soft tissues.
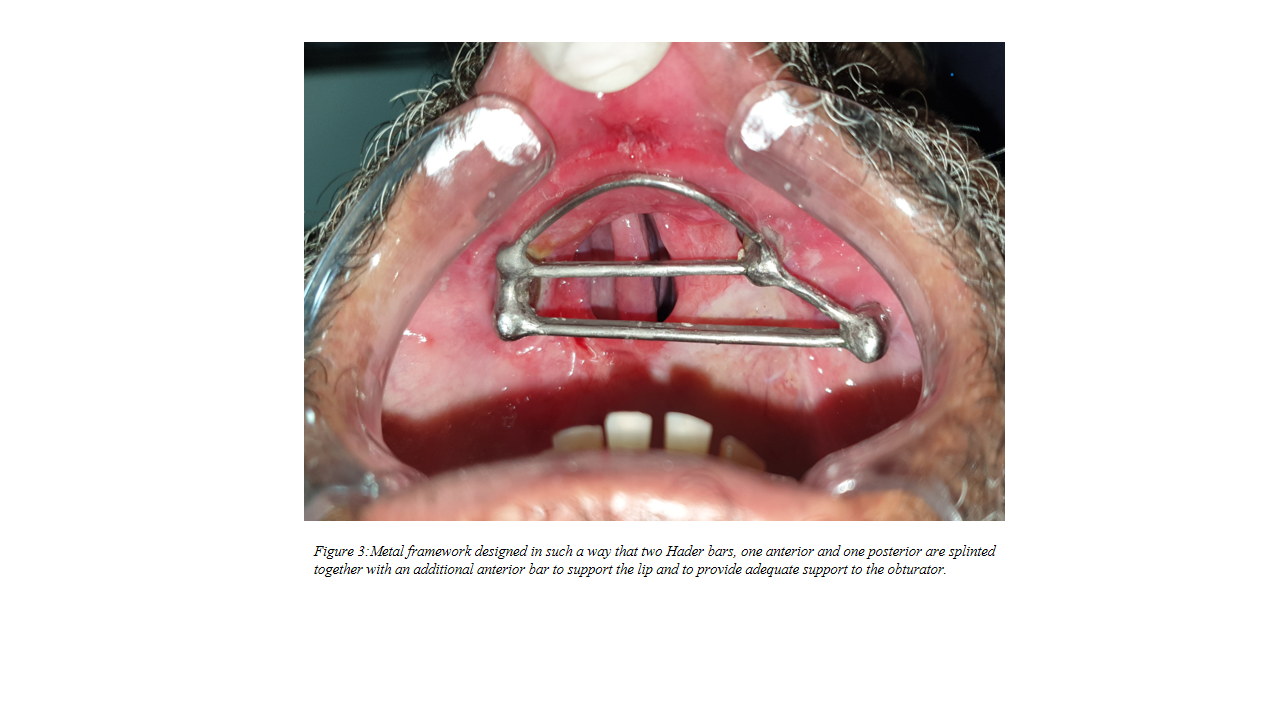
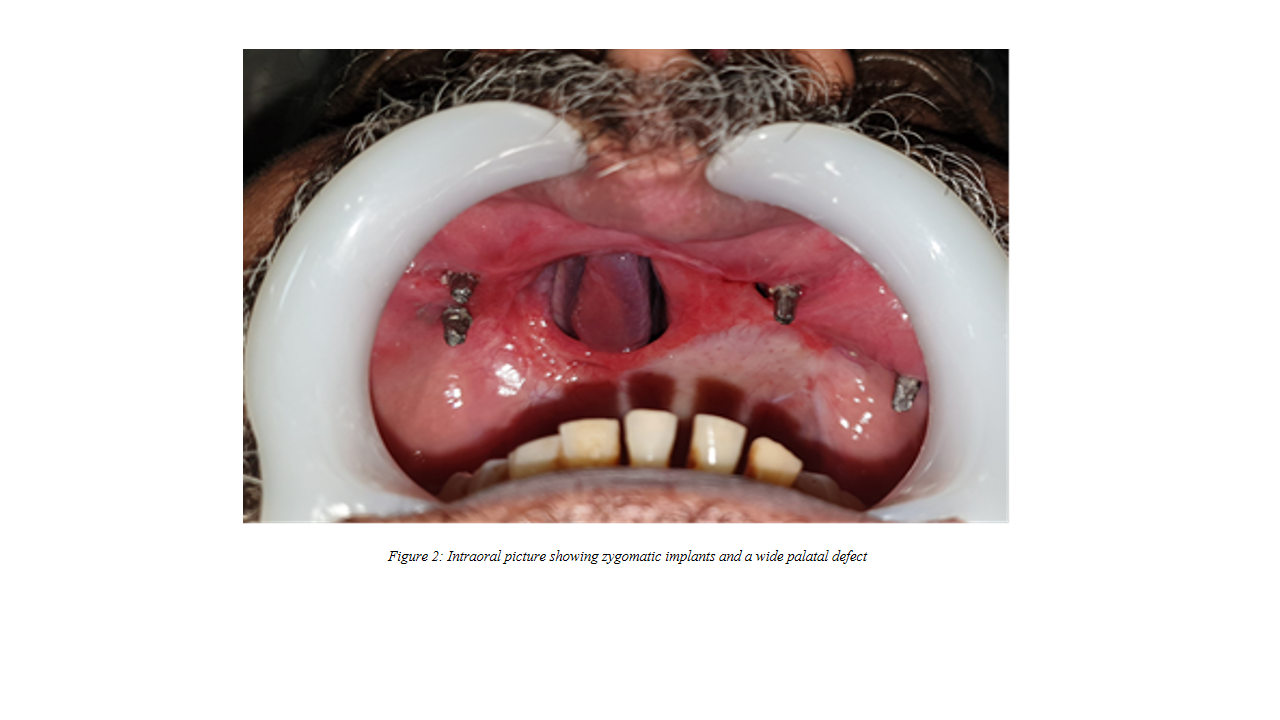
Implant size and location were planned on the basis of available bone, prosthesis design and keeping the all-on-four rehabilitation concept in consideration. Two zygomatic implants (YesBiotech Co., Ltd.) were placed in the right zygomatic bone under general anesthesia by giving a modified traditional Lefort 1 incision2 in the right lateral buccal mucosa and elevating the mucoperiosteal flap. On the left side, one zygomatic implant was placed in the zygomatic bone and one at the infraorbital rim (Figure 1 and 2). All the implants were of similar dimensions.
A previously fabricated interim prosthesis was adjusted to provide generous relief around each healing abutment such that no contact would occur during the daily function to eliminate unintentional loading. Six months were allowed for osseointegration.
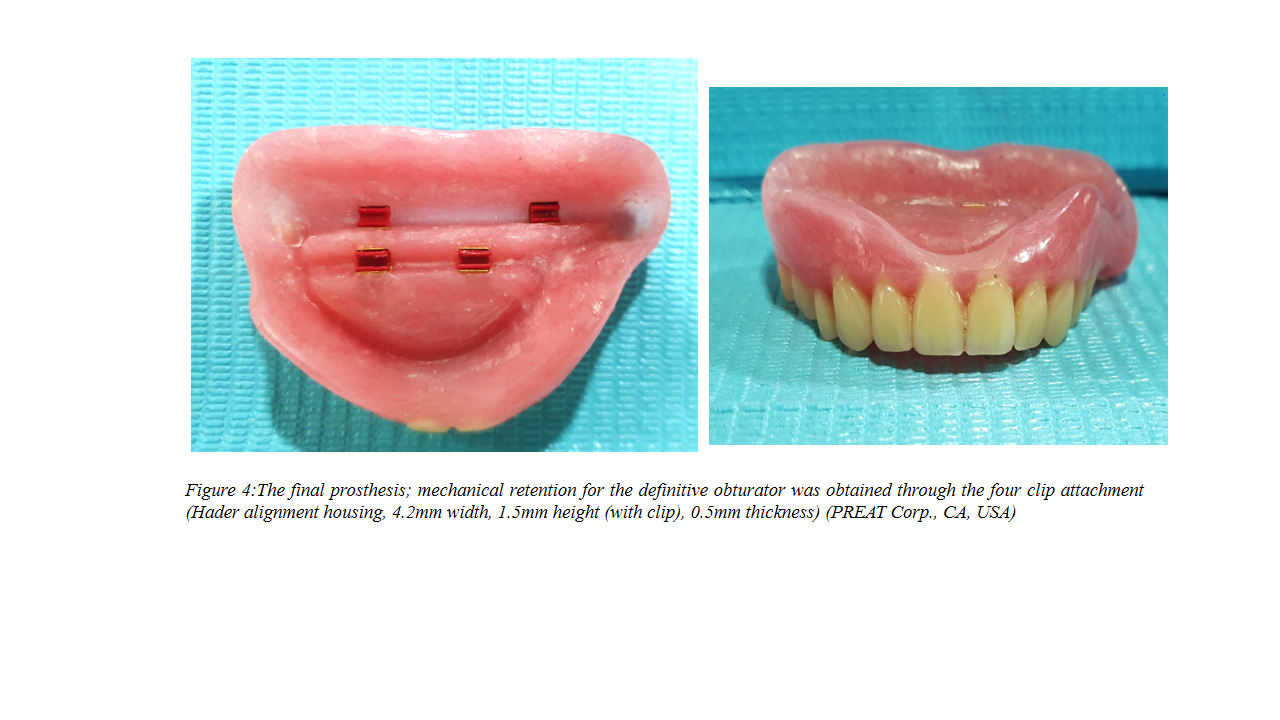
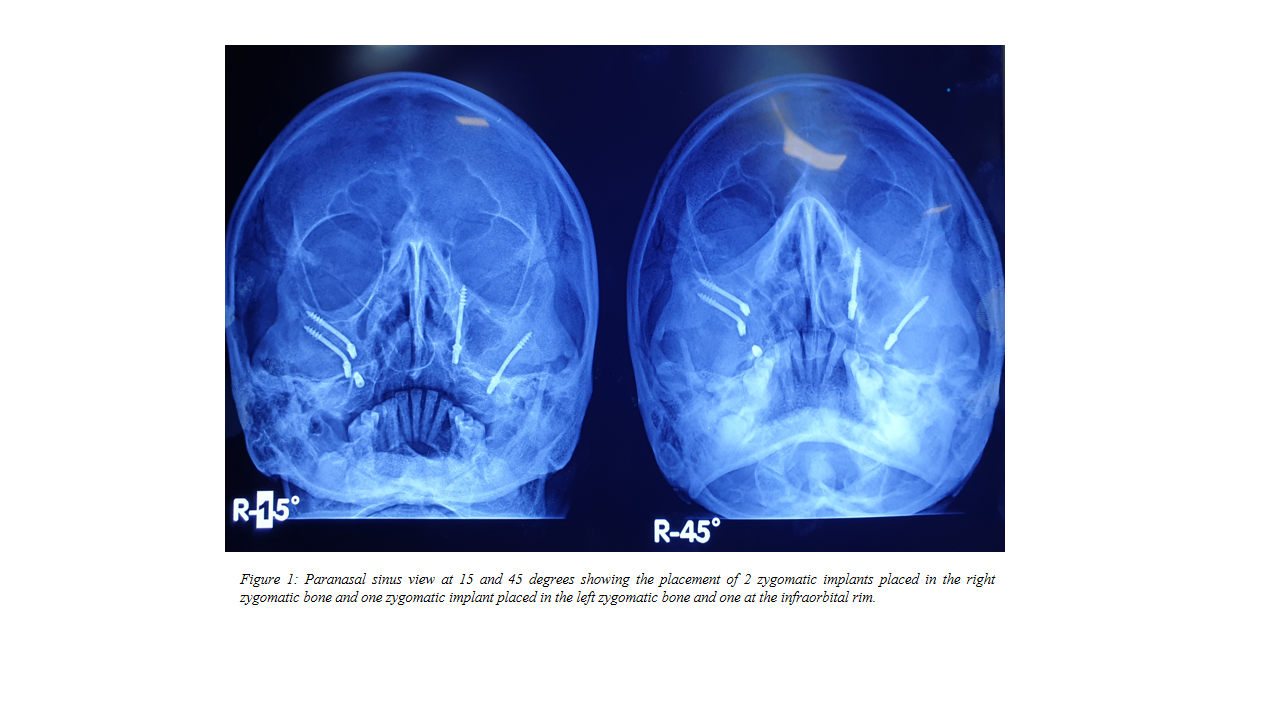
An open tray impression was made with Impregum; (3M ESPE). Further to increase the accuracy, an acrylic resin jig was fabricated for verification which was then sent to the laboratory along with the articulated cast. Instructions were given to design a customized metal framework in such a way that two Hader bars, one anterior and one posterior are splinted together with an additional anterior bar to support the lip and to provide adequate support to the obturator. The metal framework trial was carried out and found to be adequate (Figure 3). Later, a definitive obturator was fabricated. Mechanical retention for the definitive obturator was obtained through the four clip attachments (Hader alignment housing, 4.2mm width, 1.5mm height (with clip), 0.5mm thickness) (PREAT Corp., CA, USA) (Figure 4)
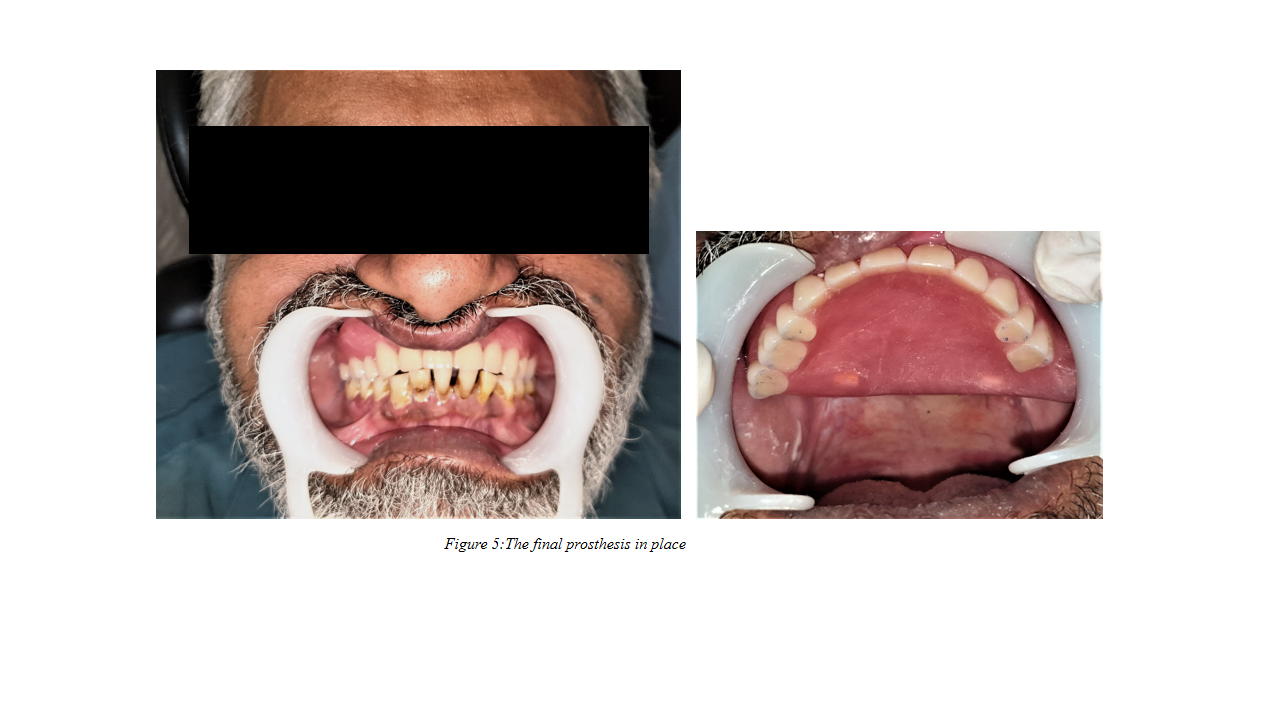
Following insertion, (Figure 5), the obturator prosthesis demonstrated optimal retention and stability which significantly improved the level of satisfaction and oral health-related quality of life of this patient. Post-insertion instructions were given with a focus on insertion, removal, and hygiene of the prosthesis.
Follow-up: The patient was recalled periodically after 1 month, 3 months, 6 months, and then annually. Few adjustments were carried out during the first 2 months of postinsertion of the prosthesis. His phonation, chewing, deglutition, and aesthetic improved significantly. Furthermore, no complications were reported or observed. The initial clip riders were replaced at 6 months and 3 years and 5 years of follow-up visits. A high level of oral health–related quality of life was obtained, demonstrating that patient satisfaction was similar to the normal population.
DISCUSSION
Various studies have shown that zygomatic implants can be used as a viable surgical option for complex and invasive osteocutaneous flap surgeries for the rehabilitation of large maxillary defects. It provides adequate retention, stability and support to the prosthesis.4The zygomatic bone has a thick cortical layer that offers a solid and extended anchorage that can bear the vertical masticatory forces.5
Literature reports that certain complications are associated with the placement of zygomatic implants, such as orbital injury/penetration, oroantral fistula formation, sensory nerve deficits temporarily, and vestibular cortical fenestration.4,5 To overcome these complications, it is crucial to plan the placement of implants on CBCT with regard to these important anatomical structures. The 12-year cumulative survival rate of zygomatic implants is 95.2% as reported in the literature,5 but clinical data regarding its long-term clinical performance is lacking. This prospective clinical case report with a 5-year follow-up period describes that zygomatic implants can be used for prosthetic rehabilitation of patients with wide maxillary defects.
CONCLUSION
The present case report provides evidence that the zygomatic implant is an excellent option to rehabilitate wide maxillary defects.
REFERENCES
1. Mittal S, Agarwal M, Chatterjee D. Rehabilitation of Posterior Maxilla with Obturator Supported by Zygomatic Implants. Case Rep Dent 2018;23;2018:3437417. https://doi.org/10.1155/2018/3437417
2. Weischer T, Schettler D, Mohr C. Titanium implants in the zygoma as retaining elements after hemimaxillectomy. Int J Oral Maxillofac Implants 1997;12(2):211-4.
3. Ali MM, Khalifa N, Alhajj MN. Quality of life and problems associated with obturators of patients with maxillectomies. Head Face Med 2018;5;14(1):2. https://doi.org/10.1186/s13005-017-0160-2
4. Ayinala M, Shetty G. Rehabilitation of Maxillary Defect Using Zygomatic Implant Retained Obturator. Case Rep Dent 2021;13;2021:2391331. https://doi.org/10.1155/2021/2391331
5. Chrcanovic BR, Albrektsson T, Wennerberg A. Survival and Complications of Zygomatic Implants: An Updated Systematic Review. J Oral MaxillofacSurg 2016;74(10):1949-64. https://doi.org/10.1016/j.joms.2016.06.166
|
AUTHORS' CONTRIBUTIONS Following authors have made substantial contributions to the manuscript as under: MSA, JA: Identification, diagnosis and management of case, drafting the manuscript, critical review, approval of the final version to be published. Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |