![]() https://doi.org/10.35845/kmuj.2024.22874 ORIGINAL
ARTICLE
https://doi.org/10.35845/kmuj.2024.22874 ORIGINAL
ARTICLE
Effects of core stability with dynamic stretching in addition to routine physical therapy in patients with chronic low back pain: a randomized controlled trial
Tanvir
Hussain 1,2,
Fareeha Amjad![]() 1,
Fahad Tanveer 1, Syed Asadullah Arsalan 1
1,
Fahad Tanveer 1, Syed Asadullah Arsalan 1
|
1: Fatima Children and Family Hospital Rana Town, Lahore, Pakistan 2: University Institute of Physical Therapy, University of Lahore, Lahore, Pakistan
Email
Contact #: +92-334-3372779
Date Submitted: June 06, 2022 Date Revised: February 27, 2024 Date Accepted: March 15, 2024 |
|
THIS ARTICLE MAY BE CITED AS: Hussain T, Amjad F, Tanveer F, Arsalan SA. Effects of core stability with dynamic stretching in addition to routine physical therapy in patients with chronic low back pain: a randomized controlled trial. Khyber Med Univ J 2024;16(2):117-22. https://doi.org/10.35845/kmuj.2024.22874 |
ABSTRACT
OBJECTIVE: To evaluate the effects of core stability with dynamic stretching along with routine physical therapy in patients with chronic low back pain (CLBP).
METHODS: This randomized controlled trial at Government Mian Munshi Hospital, Lahore, Pakistan, enrolled 48 participants with CLBP. After obtaining consent, participants were randomly assigned through lottery method to Group-A (routine physical therapy) or Group-B (routine physical therapy plus core stability exercises and dynamic stretching). Pain, range of motion (ROM), and physical disability were evaluated at pretreatment, and at 2nd, 4th, and 6th weeks post-treatment using Numeric Pain Rating Scale (NPRS), a goniometer, and Oswestry Disability Index (ODI), respectively.
RESULTS: Baseline characteristics were comparable between groups. Group-A had a mean age of 37.42±3.96 years and a mean BMI of 23.05±3.83 kg/m². Group-B had a mean age of 41.67±4.86 years and a mean BMI of 23.58±3.28 kg/m².In Group-A, the NPRS scores improved from 5.00 (4.00-7.00) to 4.00 (2.00-5.00) (p <0.001), and ODI scores improved from 40.0 (24.0-48.0) to 34.0 (14.0-35.0) (p <0.001). Flexion improved from 49.88 ± 6.955 to 53.79 ± 6.750 (p <0.001). In Group-B, the NPRS scores improved from 6.00 (4.00-7.00) to 2.80 (1.60-4.00) (p <0.001), and ODI scores improved from 46.0 (35.0-50.0) to 21.0 (30.1-28.0) (p <0.001). Flexion improved from 43.46±7.718 to 57.92±1.840 (p <0.001).
CONCLUSION: Integrating core stability exercises and dynamic stretching alongside routine physical therapy significantly improved pain intensity, physical disability, and ROM in patients with CLBP. These findings emphasize the potential benefits of these modalities as valuable adjuncts in managing CLBP.
TRIAL REGISTRATION: IRCT20210908052416N1
KEYWORDS: Exercise (MeSH); Core Stability (MeSH); Dynamic stretching (MeSH); Muscle Stretching Exercises (MeSH); Range of Motion, Articular (MeSH); Endurance (Non-MeSH); Functional movement (Non-MeSH); Low Back Pain (MeSH); Numeric pain rating scale (Non-MeSH); Pain Measurement (MeSH); Pain (MeSH); Rehabilitation (MeSH); Physical Therapy Modalities (MeSH).
INTRODUCTION
Low back pain (LBP) is a prevalent health issue affecting a significant portion of the global population, often worsening over time. It encompasses pain extending from the lowest ribs to the gluteal fold and persists for at least three months in its chronic form. LBP reduces spinal motion, impairing patients' functional capacity. 1 Its origin is non-specific in about 90% of cases, lacking a clear etiology such as rheumatological conditions, fracture, herniated discs or infections. 2 Chronic low back pain (CLBP) is a primary cause of activity restriction and job loss worldwide, imposing substantial financial burdens on individuals, families, governments, and businesses.3
Treatment for CLBP typically includes education and exercise therapy to improve muscle flexibility, coordination, endurance, and strength. Core stability exercises and dynamic stretching are integral parts of CLBP rehabilitation, aiming to enhance spinal stability, neuromuscular control, and reduce the risk of lumbar spine injuries. While many studies demonstrate their effectiveness over minimal interventions or rest, there is conflicting evidence regarding their superiority over other treatment protocols.4,5 Combined, core stability exercises and dynamic stretching have shown promising outcomes in enhancing functional ability, reducing pain, and improving thoraco-lumbar range of motion (ROM).6,7
Degenerative changes in intervertebral discs are prevalent among CLBP patients, leading to reduced spine mobility and increased load on intervertebral joints.8 This can further diminish mobility if spinal segments are affected by hypo or hypermobility.9 Muscular stretching aims to alleviate these issues by gradually extending tight muscle groups, thereby enhancing joint flexibility and reducing pain threshold, potentially through analgesic effects.10
Optimal spinal stiffness and movement depend on back muscles, which are affected by structure and injury-related pain. CLBP can cause muscle atrophy, fiber changes, fatty infiltration, and reduced strength, diminishing shock absorption and increasing lumbar compression.11,12 Muscular stretching maintains joint flexibility, enhances ROM, and reduces disability by increasing pain thresholds,13while exercise therapy effectively treats CLBP by reducing its extent and recurrence.14
The integration of core stability exercises and dynamic stretching into routine physical therapy aims to optimize outcomes in CLBP management. However, gaps persist in understanding the specific mechanisms by which these interventions improve pain intensity, physical function, and ROM compared to conventional therapies. Therefore, this study seeks to evaluate the combined effects of core stability exercises and dynamic stretching in addition to routine physical therapy on these outcomes in patients with CLBP. Such insights are essential for refining therapeutic strategies and enhancing clinical outcomes in CLBP rehabilitation.
METHODS
The study was conducted from August 2021 to May 2022 at the Physical Therapy Department of Govt. Mian Munshi Teaching Hospital in Lahore, Pakistan. Ethical approval was obtained from the Ethical Review Board of the University of Lahore (IRB-UOL-FAHS-722-v), and the study was registered with the Iranian Clinical Trial Registry (IRCT20210908052416N1).
A total of 48 participants, aged 20 to 50 years and experiencing non-specific low back pain for more than twelve weeks, were included in the study. Exclusion criteria included spondylolisthesis, cauda equina syndrome, acute trauma such as fractures within the last 6 months, cancer, and pregnancy. Participants who had received pain-mitigating treatments like injection-based therapies (e.g., epidurals) were also excluded from the study. Written informed consent was obtained from all participants prior to participation in the study.
After obtaining consent, basic personal data (name, date of birth, gender), anthropometric measurements (height, weight, BMI), history of chronic low back pain, and contact information were collected. Participants were then randomly assigned to one of two groups using the lottery method, with each group comprising 24 participants (Figure 1).
In Group-A, participants received routine physical therapy, which included 20 minutes of hot pack application and 20 minutes of traditional transcutaneous electrical nerve stimulation (TENS) to the pain site using a dual-channel portable TENS (comfy TENS 806) unit at a frequency of 80-100 HZ. Additionally, participants performed abdominal curl-ups in the supine position, back extensor exercises in the prone position, hip extensor exercises in the prone position, and lumbar rotation exercises.
In Group-B, participants were treated with core stability exercises (squats, crunches, front planks, planks with alternating leg lifts, and supine two-leg bridge exercises), dynamic stretching (slum stretch, cat and camel stretch, child pose stretch, overhead lateral stretch, and side leg swings), along with routine physical therapy. Both groups received two sessions per week for six weeks. Each session included two sets of 10-15 repetitions of each exercise. Pain intensity, range of motion, and physical disability were measured at the end of the second, fourth, and sixth weeks of treatment.
The outcome measures in this study included lumbar spine ROM, physical disability, and pain intensity. These metrics were assessed prior to the start of treatment and again at the end of the second, fourth, and sixth treatment weeks. The first outcome measure evaluated was lumbar spine ROM, which was assessed using a universal goniometer. Each participant underwent three trials of ROM measurement, with the best result being recorded. To ensure accuracy and minimize discomfort, participants were given 5-10 minutes of rest following the goniometric assessment to prevent any pain from affecting subsequent measurements.
Next, pain intensity was assessed as the second outcome measure using a Numeric Pain Rating Scale (NPRS). Participants rated the severity of their back pain on a scale from 0 to 10 and recorded it on a provided form.
The third and final outcome measure evaluated was physical disability, which was assessed using the Oswestry Disability Index (ODI) questionnaire. Participants were given adequate time to complete the questionnaire, which measures the impact of back pain on daily activities and overall functional disability.
The data were analyzed using SPSS version 20.0. Descriptive statistics were used to present quantitative variables as mean ± SD, while frequencies and percentages were used for categorical variables. Normality of the data was assessed using the Shapiro–Wilk test, revealing that the data did not meet the normality assumption. Therefore, non-parametric tests were employed for analysis.
To compare outcome measures between groups (ODI, NPRS), the Friedman test was used. For comparisons at each follow-up interval, the Mann-Whitney U test was applied. Repeated measures analysis using the Wilcoxon signed-rank test was conducted to assess changes in ODI and NPRS scores over the follow-up period, both within and between groups. A significance level of p ≤ 0.05 was considered statistically significant.
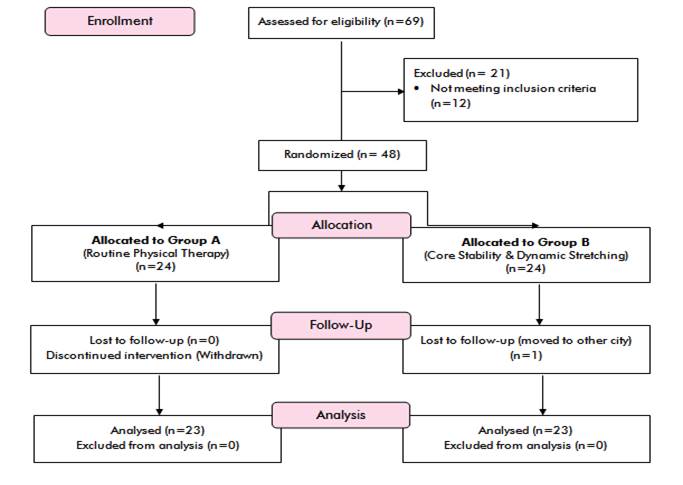
Figure 1: CONSORT flow diagram of the study
RESULTS
Patients in Group-A had a mean age of 37.42 ± 3.96 years, with age ranging from 20 to 50 years. In Group-B, the mean age was 41.67 ± 4.86 years, with ages ranging from 20 to 48 years. The mean height of patients in Group-A was 1.673 ± 0.07 meters, ranging from 1.524 to 1.92 meters, while Group-B patients had a mean height of 1.69 ± 0.08 meters, ranging from 1.554 to 1.85 meters. The mean weight for Group-A was 62.29 ± 12.11 kg, with a range of 45 to 88 kg. In Group-B, the mean weight was 64.33 ± 10.26 kg, ranging from 47 to 90 kg. The mean BMI for Group-A was 23.05 ± 3.83 kg/m², with values ranging from 17.1 to 32.3 kg/m², whereas Group-B had a mean BMI of 23.58 ± 3.28 kg/m², with a range from 17.8 to 28.1 kg/m², as shown in Table I. The data was not normally distributed, necessitating the use of non-parametric tests, as indicated by the normality test.
Table I: Demographic data of study subjects
|
Variable |
Core Stability exercise and Dynamic stretching exercise group |
Routine Physical therapy group |
||||||
|
Mean |
SD |
Mini |
Max |
Mean |
SD |
Mini |
Max |
|
|
Age(years) |
41.67 |
14.84 |
20 |
48 |
37.42 |
13.969 |
20 |
50 |
|
Height(m) |
1.673 |
0.07 |
1.524 |
1.92 |
1.695 |
0.08 |
1.554 |
1.85 |
|
Weight(kg) |
62.29 |
12.114 |
45 |
88 |
64.33 |
10.582 |
47 |
90 |
|
BMI(kg/m2) |
23.054 |
3.8235 |
17.1 |
32.3 |
23.583 |
2.8251 |
17.8 |
28.1 |
In Group-A, the pre-treatment and post-treatment values for the NPRS were 5.00 (4.00-7.00) and 4.00 (2.00-5.00), respectively (p < 0.001). For the ODI, the pre-treatment and post-treatment values were 40.0 (24.0-48.0) and 34.0 (14.0-35.0), respectively (p < 0.001). In Group-B, the pre-treatment and post-treatment NPRS values were 6.00 (4.00-7.00) and 2.80 (1.60-4.00), respectively, while the ODI values were 46.0 (35.0-50.0) and 21.0 (30.1-28.0), respectively (p < 0.001), as illustrated in Table II.
Table II: Comparison of pre and post-intervention outcome measures for the difference between the groups.
|
Variables |
Group A (Median and IQR) |
Group B (Median and IQR) |
P-value |
|
Pre-NPRS |
5.00 (4.00-7.00) |
6.00 (4.00-7.00) |
0.007 |
|
Post-NPRS |
4.00 (2.00-5.00) |
2.80 (1.60-4.00) |
|
|
Pre-ODI |
40.0 (24.0-48.0) |
46.0 (35.0-50.0) |
0.000 |
|
Post-ODI |
34.0 (14.0-35.0) |
21.0 (30.1-28.0) |
NPRS: Numeric Pain Rating Scale; ODI: Oswestry Disability Index
Pre- and post-treatment values for flexion in Group-A were 49.88 ± 6.955 and 53.79 ± 6.750, respectively, with a mean increase in flexion of 3.91 (p < 0.001). In Group-B, the pre- and post-treatment values for flexion were 43.46 ± 7.718 and 57.92 ± 1.840, respectively, with a mean increase of 14.46 (p <0.001). For extension, Group-A had pre- and post-treatment values of 19.96 ± 2.758 and 22.0 ± 2.187, respectively, with a mean increase of 2.04 (p < 0.001). In Group-B, pre- and post-treatment values for extension were 19.17 ± 2.259 and 24.21 ± 0.884, respectively, with a mean increase of 5.04 (p < 0.001).
For right lateral flexion (RLF), Group-A had pre- and post-treatment values of 20.33 ± 2.297 and 22.75 ± 1.539, respectively, with a mean increase of 2.42 (p < 0.001). In Group-B, the pre- and post-treatment values for RLF were 18.79 ± 3.050 and 23.79 ± 1.250, respectively, with a mean increase of 5.00 (p < 0.001). For left lateral flexion (LLF), Group-A had pre- and post-treatment values of 19.38 ± 2.060 and 22.46 ± 1.382, respectively, with a mean increase of 3.08 (p < 0.001). In Group-B, the pre- and post-treatment values for LLF were 19.29 ± 2.774 and 24.04 ± 1.197, respectively, with a mean increase of 4.75 (p < 0.001), as shown in Table III.
The intervention group exhibited significant improvements in physical disability, pain intensity, and ROM in this study.
Table III: Comparison of baseline and final flexion, extension, and lateral flexion degrees in groups A and B
|
Variable |
Group |
Baseline Mean ±SD |
Final value Mean±SD |
Mean change |
P value |
|
Flexion (degree) |
Group-A |
49.88±6.955 |
53.79±6.750 |
3.91 |
<.001 |
|
|
Group-B |
43.46±7.718 |
57.92±1.840 |
14.46 |
|
|
Extension (degree) |
Group-A |
19.96±2.758 |
22.0±2.187 |
2.04 |
<.001 |
|
|
Group-B |
19.17±2.259 |
24.21±0.884 |
5.04 |
|
|
Rightlateralflexion (degree) |
Group-A |
20.33±2.297 |
22.75±1.539 |
2.42 |
<.001 |
|
|
Group-B |
18.79±3.050 |
23.79±1.250 |
5.0 |
|
|
Left lateralflexion (degree) |
Group-A |
19.38±2.060 |
22.46±1.382 |
3.08 |
<.001 |
|
|
Group-B |
19.29±2.774 |
24.04±1.197 |
4.75 |
Group-A received routine physical therapy; Group-B received routine physical therapy plus core stability exercises and dynamic stretching
DISCUSSION
The study demonstrated significant improvements in key symptoms of chronic low back pain (CLBP) following six weeks of physical therapy exercises, including reduced pain, improved physical disability, and increased active back range of motion. These clinical and statistical improvements were more pronounced in the intervention group, where the p-value was less than 0.05. These findings align with research by Ebby Waqqash, who similarly found that both core stability exercises and dynamic stretching effectively alleviate pain intensity, enhance physical function, and improve thoracolumbar range of motion.15 Additionally, the intervention group in our study showed notable improvements in lumbar range of motion, consistent with findings from Baard, who observed enhanced hamstring and lumbo-pelvic-hip complex flexibility with core stability training.16
The intervention group experienced a significant reduction in pain intensity following six weeks of treatment. This finding is consistent with Waseem Akhtar's research, which highlighted the beneficial effects of core stability on reducing chronic low back pain (CLBP).17 Additionally, A. Frizziero emphasized that core stability contributes to pain reduction in LBP patients.6 Similar results were corroborated by Javadian, who observed significant pain reduction with core stability exercises in LBP treatment.18 These findings are supported by Hayden, who argued for the efficacy of core stability exercises in improving LBP.19 Furthermore, our study aligns with Brian's research, which compared core stability exercises to general exercise and found greater benefits in reducing pain and improving back-specific functional status in CLBP patients.20
Moreover, our findings suggest that core stability and dynamic stretching activities improve physical impairment in CLBP patients. Numerous studies support these outcomes, illustrating the positive impact of core stability and dynamic stretching on physical disabilities.21 Previous research has consistently integrated stabilization exercises with other types of physical activities, including stretching, strengthening, and mild aerobic exercises, highlighting their comprehensive benefits in CLBP management.19
Limitations of the study
Several limitations should be considered when interpreting the findings of this study. Firstly, the relatively small sample size of 48 participants limits the generalizability of results to a larger population. Additionally, the six-week intervention period may not fully capture the long-term sustainability of improvements or the potential for symptom recurrence. While the study employed a randomized controlled trial design, there remains a possibility of uncontrolled biases or confounding variables influencing outcomes. The study did not comprehensively monitor participant adherence to the prescribed exercise regimen, which could have affected the observed results. Furthermore, the study's focus on pain intensity, lumbar spine flexibility, and physical disability excludes broader outcomes like quality of life or psychological factors. Conducted at a single center, the study's findings may not fully reflect diverse patient demographics and clinical contexts. Addressing these limitations in future research would enhance the understanding and application of integrated therapeutic approaches for chronic low back pain management.
CONCLUSION
This study demonstrates the effectiveness of integrating core stability exercises and dynamic stretching with routine physical therapy to significantly improve outcomes in chronic low back pain patients. Participants in the intervention group experienced substantial reductions in pain intensity, enhanced lumbar spine flexibility, and decreased physical disability, highlighting the potential of integrated approaches to enhance clinical outcomes and functional capacity in this population. Moving forward, implementing this intervention program in clinical settings could markedly improve the quality of life for individuals suffering from chronic low back pain. Future research efforts should focus on further refining and optimizing these combined therapeutic strategies to better manage chronic low back pain and potentially reduce its recurrence.
REFERENCES
1. Popescu A, Lee H. Neck pain and lower back pain. Med Clin North Am 2020;104(2):279-92. https://doi.org/10.1016/j.mcna.2019.11.003
2. Malik KM, Nelson AM, Chiang TH, Imani F, Khademi SH. The specifics of non-specific low back pain: re-evaluating the current paradigm to improve patient outcomes. Anesth Pain Med 2022;12(4). https://doi.org/10.5812/aapm-131499
3. Delport E. The perspectives of Occupational Health Nurse Practitioners, employed at a National Retail Company in South Africa, regarding their management of employees with Low Back Pain. 2022. [Accessed on: January 20, 2024]. Available from URL: https://scholar.sun.ac.za/server/api/core/bitstreams/13de7c9a-22d8-42a2-90ed-632102dfb734/content
4. Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo RW, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: cochrane systematic review and meta-analysis. BMJ 2015;350:h444. https://doi.org/10.1136/bmj.h444
5. Wahyuni W, Kurnia NE. The effectiveness of core stability exercises on pain in patients with low back pain: a meta-analysis. Phys Ther J Indones 2023;4(1):85-90. https://doi.org/10.51559/ptji.v4i1.86
6. Frizziero A, Pellizzon G, Vittadini F, Bigliardi D, Costantino C. Efficacy of core stability in non-specific chronic low back pain. J Funct Morphol Kinesiol 2021;6(2):37. https://doi.org/10.3390/jfmk6020037
7. Chan EWM, Adnan R, Azmi R. Effectiveness of core stability training and dynamic stretching in rehabilitation of chronic low back pain patient. Malays J Mov Health Exerc 2019;8(1):1-13. http://dx.doi.org/10.15282/mohe.v8i1.210
8. Isa ILM, Teoh SL, Nor NHM, Mokhtar SA. Discogenic low back pain: anatomy, pathophysiology and treatments of intervertebral disc degeneration. Int J Mol Sci 2022;24(1):208. https://doi.org/10.3390/ijms24010208
9. Kulig K, Powers CM, Landel RF, Chen H, Fredericson M, Guillet M, et al. Segmental lumbar mobility in individuals with low back pain: in vivo assessment during manual and self-imposed motion using dynamic MRI. BMJ Musculoskelet Disord 2007;8:1-10. https://doi.org/10.1186/1471-2474-8-8
10. Woods K, Bishop P, Jones E. Warm-up and stretching in the prevention of muscular injury. Sports Med 2007;37(12):1089-99. https://doi.org/10.2165/00007256-200737120-00006
11. Hodges PW, Danneels L. Changes in structure and function of the back muscles in low back pain: different time points, observations, and mechanisms. J Orthops Sports Phys Ther 2019;49(6):464-76. https://doi.org/10.2519/jospt.2019.8827
12. Seif HE, Alenazi A, Hassan SM, Kachanathu SJ, Hafez AR. The effect of stretching hamstring, gastrocnemius, iliopsoas and back muscles on pain and functional activities in patients with chronic low back pain: a randomized clinical trial. Open J Ther Rehabil 2015;3(04):139-45. http://dx.doi.org/10.4236/ojtr.2015.34019
13. Büyükturan B, Şaş S, Kararti C, Büyükturan ÖJMS, Practice. The effects of combined sternocleidomastoid muscle stretching and massage on pain, disability, endurance, kinesiophobia, and range of motion in individuals with chronic neck pain: a randomized, single-blind study. Musculoskelet Sci Pract 2021;55:102417. https://doi.org/10.1016/j.msksp.2021.102417
14. Krause F, Niederer D, Banzer W, Vogt L. Medical exercise and physiotherapy modes and frequency as predictors for a recurrence of chronic non-specific low back pain. J Back Musculoskelet Rehabil 2021;34(4):665-70. https://doi.org/10.3233/bmr-200149
15. Waqqash E, Adnan R, Md Yusof S, Sulaiman N, Ismail SI, editors. Efficacy of core stability exercise and muscular stretching on chronic low-back pain. Proceedings of the International Colloquium on Sports Science, Exercise, Engineering and Technology 2014 (ICoSSEET 2014); 2014:431-9. http://dx.doi.org/10.1007/978-981-287-107-7_45
16. Baard ML, Pietersen J, van Rensburg SJ. Interventions for chronic low back pain: whole body vibration and spinal stabilisation. S Afr J Sports Med 2011;23(2):35-9. https://doi.org/10.17159/2078-516X/2011/v23i2a343
17. Bibi M, Shah A. Comparing the efficacy of core stability exercises and conventional physical therapy in the management of lower back pain: a randomized controlled trial. Northwest J Med Sci 2023;2(1)13-7.
18. Brayjani SJ, Daneshmandi H. A review of the effect of core stability exercises on pain and functional disability in people with non-specific chronic low back pain. J Paramed sci Rehabil 2021;10(1):108-18. https://doi.org/10.22038/jpsr.2021.54766.2209
19. Nambi G, Abdelbasset WK, Alqahtani BA, Alrawaili SM, Abodonya AM, Saleh AK. Isokinetic back training is more effective than core stabilization training on pain intensity and sports performances in football players with chronic low back pain: a randomized controlled trial. Medicine (Baltimore) 2020;99(21):e20418. https://doi.org/10.1097/md.0000000000020418
20. Sengul YS, Yilmaz A, Kirmizi M, Kahraman T, Kalemci OJ. Effects of stabilization exercises on disability, pain, and core stability in patients with non-specific low back pain: a randomized controlled trial. Work 2021;70(1):99-107. https://doi.org/10.3233/wor-213557
21. Buttagat V, Techakhot P, Wiriya W, Mueller M, Areeudomwong P. Effectiveness of traditional Thai self-massage combined with stretching exercises for the treatment of patients with chronic non-specific low back pain: a single-blinded randomized controlled trial. J Bodyw Mov Ther 2020;24(1):19-24. https://doi.org/10.1016/j.jbmt.2019.03.017
|
CONFLICT OF INTEREST Authors declared no conflict of interest, whether financial or otherwise, that could influence the integrity, objectivity, or validity of their research work. GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
|
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |