![]() https://doi.org/10.35845/kmuj.2024.22727 ORIGINAL ARTICLE
https://doi.org/10.35845/kmuj.2024.22727 ORIGINAL ARTICLE
Efficacy of oral versus vaginal progestogens for early pregnancy maintenance in women with recurrent miscarriages: a randomized controlled trial
|
1: Department of Obstetrics and Gynecology, Medical Teaching Institution Lady Reading Hospital, Peshawar, Pakistan 2: Department of Obstetrics & Gynecology, Kabir Medical College, Gandhara University, Peshawar, Pakistan 3: Department of Obstetrics & Gynecology, Peshawar Medical College, Peshawar, Pakistan 4: Department of Obstetrics & Gynecology, Qazi Hussain Ahmad Medical Complex, Nowshehra, Pakistan 5: Tehsil Head Quarter Hospital, Dargai, Pakistan
Email
Contact #: +92-333-9120587
Date Submitted: October 15, 2022 Date Revised: February 02, 2024 Date Accepted: March 09, 2024 |
|
THIS ARTICLE MAY BE CITED AS: Shinwari L, Aman A, Syed M, Nawaz R, Rahim R. Efficacy of oral versus vaginal progestogens for early pregnancy maintenance in women with recurrent miscarriages: A randomized controlled trial. Khyber Med Univ J 2024;16(1):25-9. https://doi.org/10.35845/kmuj.2024.22727 |
ABSTRACT
OBJECTIVE: To compare the effectiveness of oral and vaginal progestogens in the maintenance of early pregnancy in women with recurrent miscarriages.
METHODS: This randomized controlled trial was conducted at Lady Reading Hospital, Peshawar, Pakistan, from April to September 2021. Pregnant women aged 16–40 years with a history of at least three recurrent miscarriages presenting at or before 7 weeks of gestation were enrolled. A total of 108 patients were randomly assigned to two groups: group A received oral progestogens (10 mg twice daily), and group B received vaginal progestogens (200 mg twice daily). Treatment lasted for 12 weeks, with successful outcomes defined as no vaginal bleeding and pregnancy continuing beyond 12 weeks. Data analysis was conducted using SPSS-20 software.
RESULTS: The mean age of patients was 29 ± 3.88 years in group A and 27 ± 3.12 years in group B. Oral progestogens (group A) were effective in 48 (88.9%) patients, whereas vaginal progestogens (group B) were effective in 36 (66.7%) patients (p=0.03). Oral progestogens showed significantly greater efficacy compared to vaginal progestogens in individuals aged 20-30 years (p=0.04) and those with fewer than four previous miscarriages (p=0.03). However, there was no significant difference in efficacy between the two groups for participants aged 31-40 years or those with 4 or more previous miscarriages.
CONCLUSION: Oral progestogens are more effective than vaginal progestogens in preventing recurrent miscarriages, especially in participants aged 20–30 years and with fewer than 4 previous miscarriages. More research needed to validate and explore underlying mechanisms.
Clinical Trial Registration Number: IRCT20230117057148N1.
KEYWORDS: Progestins (MeSH); Fetal Viability (MeSH); Pregnancy (MeSH); Parity (MeSH); Abortion, Habitual (MeSH); Abortion, Spontaneous (MeSH).
INTRODCUTION
Recurrent miscarriage (RM) is the occurrence of three or more consecutive pregnancy losses before fetal viability, presenting a significant challenge in obstetrics and gynecology.1 It encompasses primary RM, where viable pregnancy has never been achieved, and secondary RM, characterized by a history of live births preceding miscarriages. Secondary RM typically carries a more favorable prognosis for successful pregnancy. 2-4 The prevalence of RM has been reported to range between 1% and 2%.5 In India, RM has been observed in 7.46% of women.6 Approximately 70% of pregnancies are lost before live birth: 30% due to failure to implant, 30% after implantation but before a missed period, and 10% as clinical miscarriage.7 RM complicates 15-20% of all clinically established pregnancies, with 1-2% of couples experiencing recurrent early loss.8
Despite extensive research, the pathophysiology of RM remains incompletely understood, with approximately 50% of cases lacking an identified cause. Factors such as inadequate progesterone secretion and delayed endometrial development during implantation may contribute to recurrent miscarriage.9 Various interventions, including bed rest, avoidance of sexual intercourse, uterine relaxing agents, vitamins, folic acid, human chorionic gonadotrophin, and immunotherapy, have shown ambiguous results in preventing RM.10 Progesterone therapy is commonly used to maintain early pregnancy, inducing secretory changes necessary for successful implantation. It can be administered orally, intramuscularly, rectally, or vaginally.11-13
The efficacy of progesterone therapy may be influenced by the route of administration, with minimal adverse effects associated with oral and vaginal routes compared to invasive intramuscular injections.13,14 However, controversy exists regarding the optimal route of administration, with some studies suggesting oral administration while others find no significant difference among routes.8,13 Further research is needed to evaluate the most effective route for preventing early pregnancy loss in RM. Hence, we planned this study to compare the effectiveness of oral and vaginal progestogens in the maintenance of early pregnancy in women with RM. Comparing the effectiveness of oral and vaginal progesterone may provide valuable insights for future research and potentially reduce the financial burden on patients if oral progesterone proves to be more cost-effective.
METHODS
This randomized control trial was conducted at the Post Graduate Medical Institute, Lady Reading Hospital Peshawar, Pakistan from April 2021 to September 2021. Ethical approval for this study was obtained from the Ethical Committee of the College of Physicians and Surgeons of Pakistan, reference number: CPSP/REU/OBG-2014-022-6174, dated 03-01-2020. Additionally, the study was registered with the Iranian Registry of Clinical Trials, a Primary Registry in the WHO Registry Network, under IRCTID: IRCT20230117057148N1. Total sample size calculated was 108. It was calculated using the WHO calculator: P1 proportion of effectiveness of oral progestogens 12 (A) = 87% versus P2 proportion of effectiveness of vaginal progestogens 11 (B) = 63%; power of test = 90%; 95% confidence interval; 5% level of significance; sample size was 54 in each group.
The study enrolled pregnant women aged 16–40 with a history of at least three recurrent miscarriages who presented at or before 7 weeks of gestation. Written consent was obtained from each participant after explaining the procedures, potential effects and side effects of drugs, and ensuring confidentiality. Patients with threatened miscarriage, structural uterine abnormalities distorting the cavity, absence of fetal cardiac activity (missed abortion), contraindications to progestogen use (such as allergy to progesterone or patients with breast carcinoma), chronic medical conditions (including thyroid diseases, diabetes, and hypertension), and inadequate treatment compliance were excluded from the study.
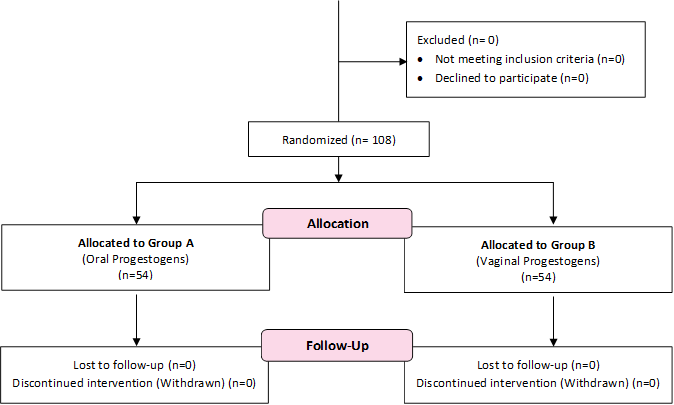
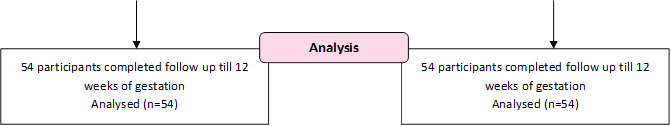
The patients were randomly divided into two equal groups, labeled as group A and group B, using computer-generated numbers. Each group comprised 54 patients. Group A received oral progestogens (dydrogesterone) at a dose of 10 mg twice daily, while group B received vaginal progestogens (micronized natural progesterone) at a dose of 200 mg twice daily for 12 weeks (Figure 1). 16 The efficacy of the treatments was assessed by the continuation of pregnancy beyond 12 weeks. All data were recorded using a pre-designed proforma. Transvaginal ultrasound examinations were conducted at 7, 9, and 12 weeks of gestation to assess the presence of fetal cardiac activity. 17
After data collection, it was entered and analyzed using SPSS 20 software. Mean and standard deviation were calculated for qualitative variables such as age. Frequency and percentage were calculated for categorical data, such as efficacy for group A and B. The efficacy of drugs between the two groups (A and B) was compared using the chi-square test. Stratification based on age and number of miscarriages was performed, and post-stratification chi-square tests were applied. A p-value ≤ 0.05 was considered significant.
Figure 1: Methodology flow diagram
RESULTS This study
was conducted on 108 women, with 54 participants in each group, to evaluate the
efficacy of oral and vaginal progestogens in preventing recurrent miscarriages
during early pregnancy. The mean age in group A was 29±3.88 years, whereas in
Group B, it was 27±3.12 years. Additional details and subdivisions concerning
age are provided in Table I. The mean age
of participants in Group A was 29±3.88 years, and in Group B, it was 27±3.12
years. The majority of participants in Group A (n=36; 66.7%) and Group B (n=38;
70.4%) belonged to the 31-40 years’ age group (Table 1). Regarding efficacy,
oral progestogens (Group A) were effective in 48 (88.9%) patients, while
vaginal progestogens (Group B) were effective in 36 (66.7%) patients (p-value =
0.03). Table I: Comparison of age distribution and
efficacy of progestogens in preventing recurrent miscarriages among study
groups A and B (n=108) Categories Group A (n=54) Group B (n=54) p-value Age (years) 20-30 18 (33.3%) 16 (29.6%) 0.67 31-40 36 (66.7%) 38 (70.4%) Efficacy Effective 48 (88.9%) 36 (66.7%) 0.03 Not Effective 6 (11.1%) 18 (33.3%) Group A: received oral progestogens; Group
B received vaginal progestogens
Table II
illustrates the comparison of oral and vaginal progestogens' efficacy in
preventing recurrent miscarriages based on age and the number of previous miscarriages.
Oral progestogens showed significantly higher efficacy than vaginal
progestogens in participants aged 20-30 years (p=0.04) and those with fewer
than 4 previous miscarriages (p=0.03). No significant difference was observed
in efficacy between the two groups for participants aged 31-40 years or those
with 4 or more previous miscarriages. Table II: Comparison of efficacy of oral
and vaginal progestogens in preventing recurrent miscarriages based on age and
number of previous miscarriages Variables Efficacy Group A (n=54) Group B (n=54) P Value# Age
(years) 20-30 Effective 17
(31.5%) 7 (13%) 0.04 Not effective 1
(1.9%) 6 (11.1%) 31-40 Effective 31 (57.4%) 29 (53.7%) 0.18 Not effective 5 (9.2%) 12 (22.2%) No.
of miscarriage ≤ 4 Effective
44 (81.5%) 27 (50%) 0.03 Not
effective 2 (3.7%) 10 (18.5%) ≥4 Effective
4 (7.4%) 9 (16.7%) 0.36 Not
effective 4 (7.4%) 8 (14.8%) Group A:
received oral progestogens; Group B received vaginal progestogens #
Chi-square test DISCUSSION The
current study aimed to assess the effectiveness of progesterone via oral and
vaginal routes. Our findings indicate that treatment with oral progestogens was
significantly more effective in preventing RM compared to vaginal progestogens
(p < 0.05). Stratification by age and number of miscarriages also revealed
significant differences in efficacy between the groups (p < 0.05). Progesterone,
often referred to as the "pregnancy hormone," plays a crucial role in
facilitating the successful implantation of a fertilized egg into the uterine
lining. Beyond this primary function, progesterone also contributes to various
processes, including the suppression of inflammatory responses, modulation of
maternal immune responses, reduction of uterine contractility, support during
the luteal phase, and enhancement of utero-placental circulation.15
It is suggested that inadequate secretion of progesterone may be a contributing
factor in many cases of miscarriages. As a result, gynecologists and
obstetricians frequently administer progesterone during the first trimester of
pregnancy to prevent spontaneous miscarriage.18 Various
studies have been conducted to investigate the role of progesterone in maintaining
pregnancy, particularly in cases of threatened and recurrent miscarriages.19,20 However, controversy persists
regarding the optimal route of administration, as evidenced by conflicting
results in existing research.8,13 In our study, oral progestogens
demonstrated superior efficacy, consistent with findings from other research.16
A study reported by Ghosh et al.,21 in 2014 found oral progesterone
(10mg BID) effective in 90% of cases, aligning with our results. Additionally,
Ghosh et al., observed higher pregnancy rates (92.0%) in the oral progestogens
group compared to the vaginal progestogens group (82.3%). Similarly, Wang et
al.,22 reported a lower risk of miscarriage in women treated with
oral progestogens compared to those receiving vaginal progestogens. A
meta-analysis by Wahabi et al.,23 further supported the superiority
of oral progestogens in reducing the incidence of recurrent miscarriages during
pregnancy. A
review conducted by a group of obstetricians and gynecologists in Saudi Arabia
emphasized the role and route of progestogens in preventing recurrent
miscarriage. Their analysis concluded that oral progestogens were well
tolerated and more effective in reducing the risk of recurrent miscarriage in
at-risk women.8 Another study by El-Zebdeh and colleagues
investigated the effect of oral progestogens in recurrent miscarriage and found
that viable pregnancies occurred in 87% of cases beyond 12 weeks.24
These findings align with the results of our study and are consistent with the
majority of the aforementioned studies. In
contrast, Lee et al.,25 conducted a systematic review encompassing
51 articles, comparing the efficacy of oral and vaginal progestogens in
preventing RM. While they found no significant difference in the efficacies of
oral and vaginal progestogens when compared individually, oral progestogens
were slightly more effective than vaginal progestogens when compared to the
control group. Similarly, Barbosa et al.13 conducted another
systematic review comparing the efficacy of the two routes in preventing
miscarriage. Their analysis concluded that there was no significant difference
in miscarriage rates between oral and vaginal progestogens. Additionally, both
routes showed similar outcomes in terms of ongoing pregnancies/live births. The
effective role of progesterone in maintaining pregnancy may be attributed to
its fundamental role in various reproductive processes. Progesterone
facilitates secretory changes in the uterine lining, which are crucial for
successful embryo implantation. Additionally, progesterone reduces uterine
contractility, further supporting the implantation process.20
Progesterone is also thought to regulate the mother's immune responses,
preventing rejection of the embryo. Furthermore, pro-inflammatory cytokines
have been linked to miscarriage frequency, while progesterone-induced blocking
factor suppresses immunological reactions and promotes a shift from type-1 to
type-2 cytokines, ultimately increasing type-2 cytokine levels.26 CONCLUSION In conclusion, oral progestogens demonstrate superior
efficacy over vaginal progestogens in preventing recurrent miscarriages during
early pregnancy. This was evidenced by significantly higher effectiveness rates
in the oral progestogens group (88%), compared to the vaginal progestogens
group (66%). An important finding of our study was the greater efficacy of oral
progestogens among participants aged 20–30 years and those with fewer than 4
previous miscarriages. These results highlight the significance of considering
the route of administration when prescribing progestogens to prevent recurrent
miscarriages. Further research may be necessary to validate these results and
explore the underlying mechanisms. REFERENCES
1. Regan L, Rai R, Saravelos S, Li TC; Royal College of
Obstetricians and Gynaecologists. Recurrent Miscarriage Green-top Guideline No.
17. Br J Obstetrics Gynecol. 2023 Nov;130(12):e9-e39. https://doi.org/10.1111/1471-0528.17515. 2. Linehan LA, San Lazaro Campillo I, Hennessy M, Flannery
C, O’Donoghue K. Reproductive outcomes following recurrent first-trimester
miscarriage: a retrospective cohort study. Hum
Reprod Open 2022;2022(4):hoac045. https://doi.org/10.1093/hropen/hoac045 3. Navya G, Raghuwanshi N, Chavan R. Clinico-epidemiological
profile and evidence based management of recurrent miscarriages in a tertiary
care centre. Int. J. of Adv. Res. 2023; 11(05):613-627. https://www.journalijar.com/article/44810/ 4.
Ali S, Majid S, Ali NM, Taing S, El-Serehy HA, Al-Misned FA.
Evaluation of etiology and pregnancy outcome in recurrent miscarriage patients.
Saudi J Biol Sci 2020;27(10):2809-17. https://doi.org/10.1016/j.sjbs.2020.06.049 5.
Tsonis O, Balogun S, Adjei JO, Mogekwu O, Iliodromiti S.
Management of recurrent miscarriages: an overview of current evidence. Curr
Opin Obstet Gynecol 2021;33(5):370-7. https://doi.org/10.1097/GCO.0000000000000735. 6.
Patki A., Chauhan N. An epidemiology study to determine the
prevalence and risk factors associated with recurrent spontaneous miscarriage
in India. J. Obstet. Gynecol. India., 66 (2016), pp. 310-315, https://doi.org/10.1007/s13224-015-0682-0 7.
Barnhart KT, Katz I, Hummel A, Gracia CR. Presumed diagnosis of
ectopic pregnancy. Obstet Gynecol 2002;100(3):505-10. https://doi.org/10.1016/S0029-7844(02)02142-7 8. Arab H, Alharbi AJ, Oraif A, Sagr E, Al Madani H,
Abduljabbar H, et al. The role of progestogens in threatened and idiopathic
recurrent miscarriage. Int J Womens Health 2019;11:589-96. https://doi.org/10.2147/IJWH.S224159 10. Nelson DB, Hanlon AL, Wu G, Liu C, Fredricks DN. First
trimester levels of BV-associated bacteria and risk of miscarriage among women
early in pregnancy. Matern Child Health J 2015;19(12):2682-7. https://doi.org/10.1007/s10995-015-1790-2 11. Giakoumelou S, Wheelhouse N, Cuschieri K, Entrican G,
Howie SE, Horne AW. The role of infection in miscarriage. Hum Reprod Update
2016;22(1):116‐33. https://doi.org/10.1093/humupd/dmv041 12. Thangaratinam S, Tan A, Knox E. Association between
thyroid autoantibodies and miscarriage and preterm birth: meta-analysis of
evidence. BMJ 2011;342:d2616. https://doi.org/10.1136/bmj.d2616 16. Abrar S, Abrar T, Tahir M, Sayyed E. Efficacy of oral
with vaginal progesterone in the treatment of threatened miscarriage in first
trimester. Pak J Med Sci 2017;25(4):407-10. https://doi.org/10.12669/pjms.37.3.3700 17. Di Renzo GC, Giardina, I, Clerici G, Brillo E, Gerli S.
Progesterone in normal and pathological pregnancy. Hor Mol Bio Clin Investig
2016;27(1):35-48. https://doi.org/10.1515/hmbci-2016-0038 18. Schumacher A, Costa SD, Zenclussen AC. Endocrine factors
modulating immune responses in pregnancy. Front Immunol 2014;5:196. https://doi.org/10.3389/fimmu.2014.00196 19. Yassaee F, Shekarriz-Foumani R, Afsari S, Fallahian M.
The effect of progesterone suppositories on threatened abortion: A randomized
clinical trial. J Reprod Infertil 2014;15(3):147-51. 20. Dante G, Vaccaro V, Facchinetti F. Use of progestagens
during early pregnancy. Facts Views Vis Obgyn 2013;5(1):66-71. 21. Ghosh S, Chattopadhyay R, Goswami S, Chaudhury K,
Chakravarty B, Ganesh A. Assessment of sub-endometrial blood flow parameters
following dydrogesterone and micronized vaginal progesterone administration in women
with idiopathic recurrent miscarriage: a pilot study. J Obstet Gynaecol Res
2014;40(7):1871‐6. https://doi.org/10.1111/jog.12456 22. Wang XX, Luo Q, Bai WP. Efficacy of progesterone on
threatened miscarriage: difference in drug types. J Obstet Gynaecol Res
2019;45(4):794-802. https://doi.org/10.1111/jog.13909 23. Wahabi H, Fayed A, Esmaeil A, Al-Zeidan A. Progestogen
for treating threatened miscarriage. The Cochrane Database of Systematic
Reviews 2011;12:CD005943.005943. https://doi.org/10.1002/14651858.CD005943.pub5 24. El-Zibdeh MY, Yousef LT. Dydrogesterone support in
threatened miscarriage. Maturitas 2009;65(1):S43-6. https://doi.org/10.1016/j.maturitas.2009.11.013 25. Lee HJ, Park TC, Kim JH, Norwitz E, Lee B. The Influence
of Oral Dydrogesterone and Vaginal Progesterone on Threatened Abortion: A
Systematic Review and Meta-Analysis. Biomed Res Int 2017;3616875. https://doi.org/10.1155/2017/3616875 26. Kasap E, Karaarslan S, Gene M, Gur EB, Sahin N, Guclu S.
The role of cytokines in first trimester pregnancy losses with fetal
chromosomal anomaly. Ginekol Pol 2015;86(11):827-32. CONFLICT OF INTEREST Authors
declared no conflict of interest, whether financial or otherwise, that could influence
the integrity, objectivity, or validity of their research work. GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors
declared no specific grant for this research from any funding agency in the
public, commercial or non-profit sectors DATA SHARING STATEMENT The data that support the findings of this
study are available from the corresponding author upon reasonable request KMUJ
web address: www.kmuj.kmu.edu.pk Email
address: kmuj@kmu.edu.pk
![]()
![]()
![]() This is an Open Access article
distributed under the terms of the Creative Commons
Attribution-Non-Commercial 2.0 Generic License.
This is an Open Access article
distributed under the terms of the Creative Commons
Attribution-Non-Commercial 2.0 Generic License.