![]() https://doi.org/10.35845/kmuj.2023.21908
ORIGINAL ARTICLE
https://doi.org/10.35845/kmuj.2023.21908
ORIGINAL ARTICLE
Diagnostic accuracy of plain magnetic resonance imaging of cruciate ligaments and meniscal injuries keeping arthroscopy as gold standard
QaziShahrukh1, Osama
Sherjeel Khan 1, Qaisar Azim 1 ![]() , Ahmad Jawad Mufti 1, Zahid Askar1
, Ahmad Jawad Mufti 1, Zahid Askar1
|
1: Department of Orthopaedic and Trauma, Khyber Teaching Hospital Medical Teaching Institution, Peshawar, Pakistan
Email
Contact #: +92-300-9095986
Date Submitted: August 16, 2021 Date Revised: February 27, 2023 Date Accepted: March 10, 2023 |
|
THIS ARTICLE MAY BE CITED AS: Shahrukh Q, Khan OS, Azim Q, Mufti AJ, Askar Z. Diagnostic accuracy of plain Magnetic Resonance Imaging of cruciate ligaments and meniscal injuries keeping arthroscopy as gold standard. Khyber Med Univ J 2023;15(1):44-8. https://doi.org/10.35845/kmuj.2023.21908 |
ABSTRACT
OBJECTIVE: To find out the accuracy of plain Magnetic Resonance imaging (MRI) in comparison with arthroscopy in diagnosing cruciate ligaments and meniscal injuries.
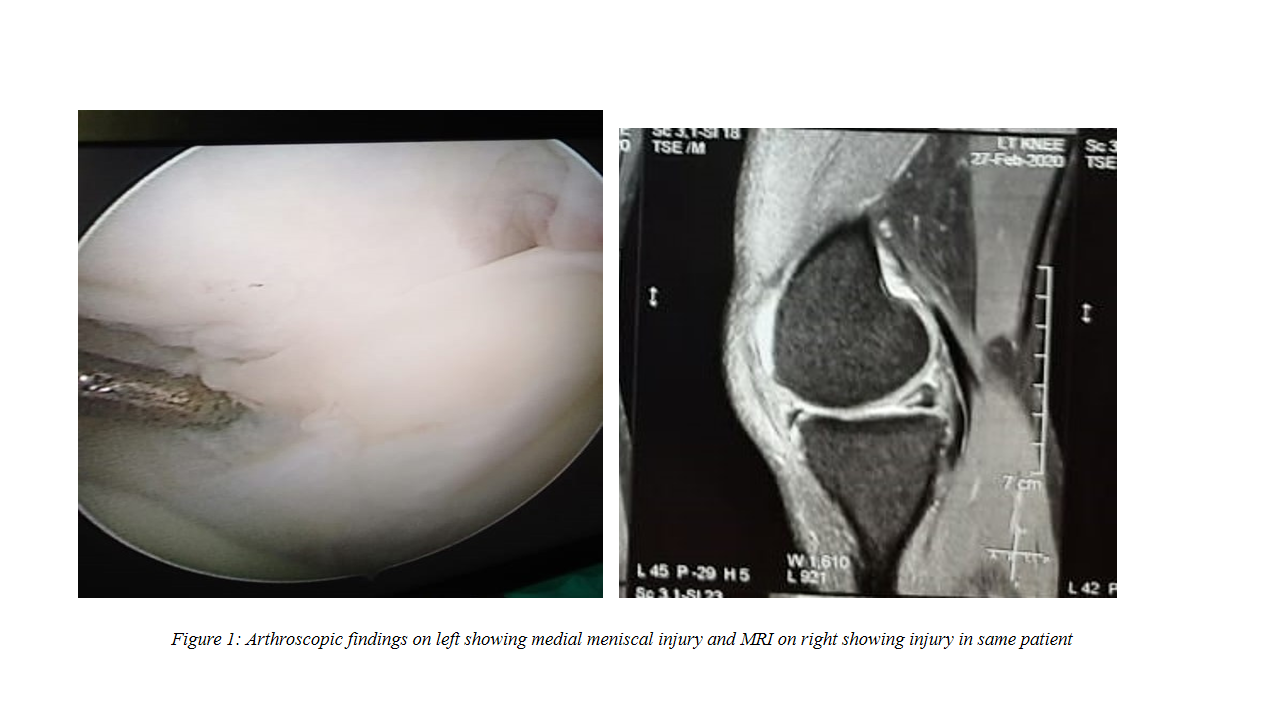
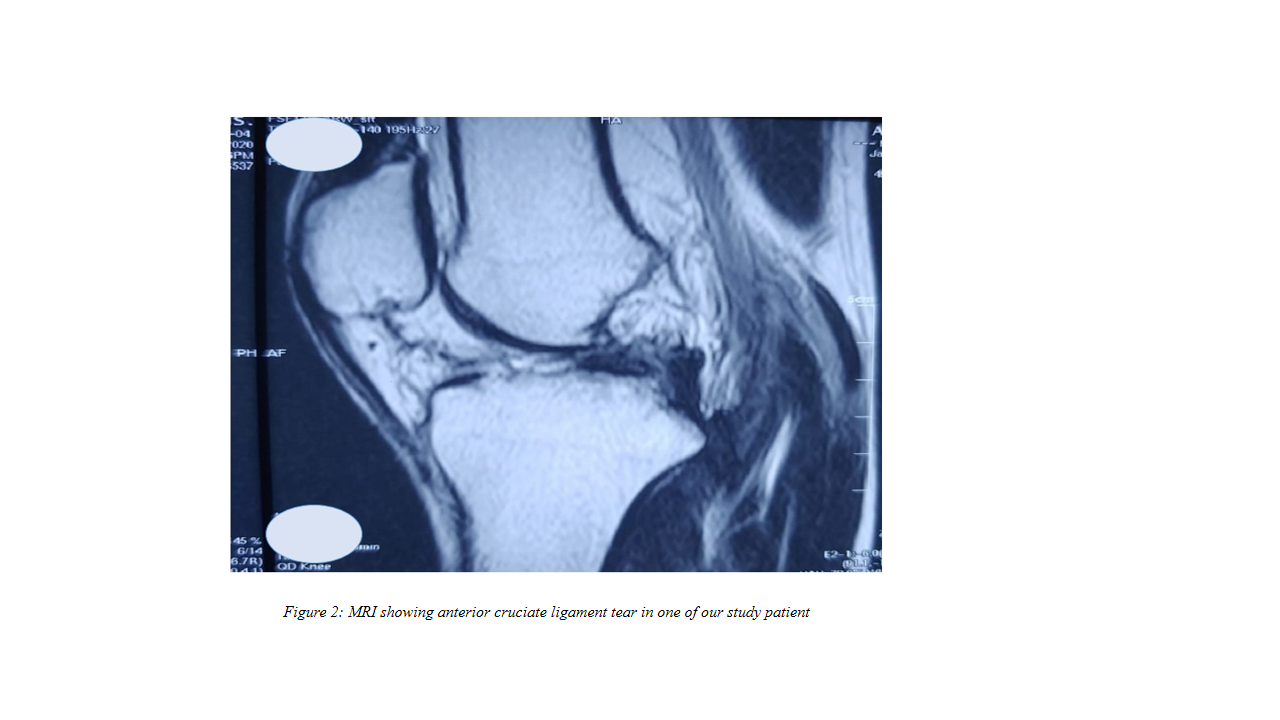
METHODS: This prospective study was conducted from June 2019 to June 2020 at Khyber Teaching Hospital Peshawar, Pakistan. All patients, aging 14-55 years, with history of trauma to knee and suspected meniscal and ligament injuries were included. Patients with positive findings on clinical examination and MRI were sent for arthroscopy. Findings on MRI and arthroscopy were compared for diagnostic accuracy.
RESULTS: Out of 100 patients, 87 were males. Fifty-nine patients had anterior cruciate ligament injuries (ACLI), one patient had posterior cruciate ligament injuries (PCLI), 49 patients had medial meniscus injuries (MMI) and 8 had lateral meniscal injuries (LMI) respectively. Sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of MRI was 93.4%, 71.4%, 82.35% & 88.23% respectively for ACLI and 100%,96%,20% and 100%respectively for PCLI. Similarly, sensitivity, specificity, PPV and NPV of MRI was 81.6%, 45.3%, 57.97%& 72.72%respectively for MMI and 37.5%, 91.5%, 27.27% and 94.5%respectively for LMI. There was no statistically significant difference for gender (p=0.43) and side of knee (p=0.22) between MRI vs arthroscopy.
CONCLUSION: MRI has high sensitivity and NPV for ACLI & PCLI, low sensitivity for LMI, low specificity for MMI and low PPV for PCLI, MMI and LMI. In cases of clinical suspicion of meniscal or ligamental injury, clinicians should not rely on MRI findings alone but should follow it up with diagnostic arthroscopy.
KEYWORDS: Knee (MeSH); Anterior Cruciate Ligament (MeSH); Posterior Cruciate Ligament (MeSH); Meniscus (MeSH); Diagnostic Imaging (MeSH); Magnetic Resonance Imaging (MeSH); MRI Knee (Non-MeSH), Arthroscopy (MeSH); Knee Injuries (MeSH);Menisci, Tibial (MeSH).
INTRODUCTION
Anterior Cruciate ligament (ACL) ruptures of the knee have a prevalence of 1 in 3500 people per year making them the most common ligament injury.1 The typical injury pattern flexion with a valgus stress and external rotation.2 Typical associations of this injury pattern also include medial collateral ligament ruptures, posterior horn of medial meniscal tears.3
A ruptured ACL leads to knee joint instability in the anteromedial direction, with anterior translocation of the tibia over the femur. There is increased stress on the menisci which act as primary stabilizers against this movement and increased damage to articular cartilage chronically. Secondary injuries to the meniscus have been associated with ACL tears in around 30 % of these patients. 4,5
The gold standard in the diagnosis of ligamentous injuries of the knee is widely considered to be the Magnetic Resonance imaging (MRI), and has achieved widespread popularity. Literature reports the sensitivity of MRI for ACL tears between 80-100%.6,7 False negative findings in MRI are however still possible due to difficulties in interpretation and inter-observer variation. Various other possible sources of error have been hypothesized and lase negative findings may approach 20%. 7
Arthroscopy of the knee has a reported accuracy of as high as 95-98% in the diagnosis of soft tissue knee injuries secondary to trauma.8 This technique, is however more invasive, expensive and time consuming than an MRI and may lead to other potential complications. 9
The rationale of the study revolves around a multi-factorial intent. One of the most important was to correlate local data with international studies. Also our study was to emphasize on the fact whether one can proceed to arthroscopy directly after clinical examination without MRI of the knee joint involved. This would also give a positive economic impact in terms of the population where study is done. Our plan in the study was to compare the diagnostic accuracy of MRI keeping arthroscopy as the conventional standard in the evaluation of ligamentous and meniscal injuries.
METHODS
This prospective study was conducted from June 2019 to June 2020 in of orthopaedics and trauma, Khyber teaching hospital Peshawar, Pakistan. All the patients were received in outpatient department and after thorough history and physical examinations, consent was taken from the patient for inclusion in the study and for interventions ordered, they were advised MRI. Then depending upon the MRI reports given by experienced radiologist, decision was taken whether to proceed with arthroscopy or not. Experienced radiologist included an Assistant Professor by designation with minimum 5 years of experience. Multiple radiologists were not consulted to reduce bias. If arthroscopy was performed, then the findings or MRI and arthroscopy were compared. All patients with history of trauma to the knee and suspected meniscal and ligament injuries of age 14-55 years were included. Patients with associated bony injuries like femur condyle or tibial plateau fractures were excluded from the study. Grading was not done because patients with clinical symptoms un-resolving with conservative treatment were ordered for MRI. All patients with positive clinical findings and positive findings on MRI were sent for arthroscopy. There were no negative MRIs included in the study. Other exclusions included patients with history of previous surgeries to the knee and those in whom MRI was contraindicated. After arthroscopy was done and findings noted, the sensitivity, specificity along with the positive and negative predictive values were calculated.
This study was a cross-sectional study and no patient follow up was included in the study. The study was approved by Institutional Review Board (IREB).
MRI technique: Clinically we ordered MRI for patients who had symptoms and had positive signs on clinical examination. After obtaining informed consent, the patient was placed supine on the MRI table. The knee was positioned in extension and 15 degrees of external rotation. A 1.5 tesla MRI machine was used using coronal T2 FSE, coronal PD FATSAR and axial STIR sequences. The obtained digital images were assessed by a radiologist who was unaware of the patient and provisional diagnosis. The ACL was assessed on all available images and categorized as intact or torn. An intact ACL was described as a hypointense band seen in the anatomical location, without appearance of a discontinuity, abnormal signal intensity or poor definition. A meniscus which was hypodense with no altered signal intensity was considered normal.
Arthroscopic examination:after complete preoperative preparation and informed consent, the arthroscopies were performed under spinal anaesthesia. All procedures were performed by a single orthopaedic surgeon. A systematic and thorough examination of all compartments i.e. the suprapatellar pouch, patellofemoral joint, medial gutter, medial compartment intercondylar notch, posteromedial compartment, lateral compartment, lateral gutter and posterolateral compartment was done. On identification of the tear, appropriate surgical intervention was done, i.e. ACL reconstruction, meniscectomy or meniscal repair.
True and false positives and negatives were determined by comparing arthroscopic with MRI findings. Comparable positive MRI and arthroscopy findings were labelled as true positive, while comparable negative MRI and arthroscopic findings were labelled as true negative. A negative arthroscopy after a positive MRI were labelled as false positive while positive arthroscopies after a negative MRI were labelled as false negative. SPSS v.20 was used for analysis of all data in this study.
RESULTS
Out of 100 patients of knee injuries with both MRI and arthroscopic findings 87 patients were male and 13 were female. Out of these patients, 48 had injuries to the right knee while 54 had injuries to the left knee with 2 patients having bilateral knee involvement hence number of knees injured being 102 for 100 patients. By involvement of types of ligament (n=118), we observed that most commonly affected ligament was the anterior cruciate ligament (n=60/102; 58.82%) followed by medial meniscus (n=49/102; 48.04%), lateral meniscus (n=8/102, 7.84%) and posterior cruciate ligament being the least affected (n=1/102, 0.98%).
The correlation of MRI findings with arthroscopic findings was done in 100 patients and was categorized into true positive (TP), true negative (TN), false positive (FP) and false negative (FN) cases. Sensitivity, specificity, positive predictive value (PPV) and negative predictive (NPV) value of MRI was calculated separately for each ligament and menisci involved.
Correlation between MRI and arthroscopic findings for injuries of anterior cruciate ligament (ACL) is given in Table I. TP, TN, FP and FN cases for injuries of ACL on MRI were 56; 30, 12 and 4 respectively. MRI for knee joint had a sensitivity of 93.4%, specificity of 71.4%, PPV of 82.35% and NPV of 88.23% in terms of ACL injury assessment (Table 1).
Table I: DEMONSTRATING A CORRELATION BETWEEN MRI AND ARTHROSCOPIC FINDINGS FOR INJURIES OF ANTERIOR CRUCIATE LIGAMENT
|
|
Arthroscopy Findings |
|||
|
Yes |
No |
Total |
||
|
Magnetic Resonance Imaging (MRI) Findings |
Yes |
56 (93.3%)
|
12 (28.6%)
|
68 (66.7%) |
|
No |
4 (6.7%)
|
30 (71.4%)
|
34 (33.3%) |
|
|
Total |
60 (100%) |
42 (100%) |
102 (100%) |
|
Sensitivity= 93.4%, Specificity= 71.4%, Positive Predictive Value=82.35%, Negative Predictive Value=88.23%
Correlation between MRI and arthroscopic findings for injuries of posterior cruciate ligament (PCL) is given in Table II. TP, TN, FP and FN cases for injuries of PCL on MRI were 1, 97, 4 and 0 respectively. MRI for knee joint had a sensitivity of 100%, specificity of 96%, PPV of 20% and NPV of 100% in terms of PCL injury assessment (Table II).
Table II: DEMONSTRATING A CORRELATION BETWEEN MRI AND ARTHROSCOPIC FINDINGS FOR INJURIES OF POSTERIOR CRUCIATE LIGAMENT
|
|
Arthroscopy Findings |
|||
|
Yes |
No |
Total |
||
|
Magnetic Resonance Imaging (MRI) Findings |
Yes |
1 (100.0%) |
4 (4.0%) |
5 (4.9%) |
|
No |
0 (0.0%) |
97 (96.0%) |
97 (95.1%) |
|
|
Total |
1 (100.0%) |
101 (100.0%) |
102 (100.0%) |
|
Sensitivity= 100%, Specificity= 96%, Positive Predictive Value=20%, Negative Predictive Value=100%
Correlation between MRI and arthroscopic findings for injuries of medial meniscus is given in Table III. TP, TN, FP & FN cases for injuries of medial meniscus on MRI were 40, 24, 29 & 9 respectively. MRI for knee joint had a sensitivity of 81.6%, specificity of 45.3%, PPV of 57.97% and NPV of 72.72% in terms of medial meniscus injury assessment (Table III).
Table III: DEMONSTRATING A CORRELATION BETWEEN MRI AND ARTHROSCOPIC FINDINGS FOR INJURIES OF MEDIAL MENISCUS
|
|
Arthroscopy Findings |
|||
|
Yes |
No |
Total |
||
|
Magnetic Resonance Imaging (MRI) Findings |
Yes |
40 (81.6%) |
29 (54.7%) |
69 (67.6%) |
|
No |
9 (18.4%) |
24 (45.3%) |
33 (32.4%) |
|
|
Total |
49 (100.0%) |
53 (100.0%) |
102 (100.0%) |
|
Sensitivity= 81.6%, Specificity= 45.3%, Positive Predictive Value=57.97%, Negative Predictive Value=72.72%
Correlation between MRI and arthroscopic findings for injuries of lateral meniscus is given in Table IV. TP, TN, FP & FN cases for injuries of medial meniscus on MRI were 3, 86, 8 & 5 respectively. MRI for knee joint had a sensitivity of 37.5%, specificity of 91.5%, PPV of 27.27% and NPV of 94.5% in terms of lateral meniscus injury assessment (Table IV).
There was no statistically significant correlation between the gender (p=0.43) and side of knee (p=0.22) with the accuracy of MRI vs arthroscopy.
Table IV: DEMONSTRATING A CORRELATION BETWEEN MRI AND ARTHROSCOPIC FINDINGS FOR INJURIES OF LATERAL MENISCUS
|
|
Arthroscopy Findings |
|||
|
Yes |
No |
Total |
||
|
Magnetic Resonance Imaging (MRI) Findings |
Yes |
3 (37.5%) |
8 (8.5%) |
11 (10.8%) |
|
No |
5 (62.5%) |
86 (91.5%) |
91 (89.2%) |
|
|
Total |
8 (100.0%) |
94 (100.0%) |
102 (100.0%) |
|
Sensitivity= 37.5%, Specificity= 91.5%, Positive Predictive Value=27.27%, Negative Predictive Value=94.5%
DISCUSSION
Our study showed a variable but low false positive result when reported in all kinds of injuries studied. Patients were labelled as false positive when they were described as having tear on MR report but were found to not have any tear on arthroscopy. Two explanations have been given for these high false positive errors on medial meniscus tears. First one being; a healed tear can’t be differentiated from an acute tear on MR imaging as reported in one of the previous studies done.10 Second explanation was given by Quinn and Brown who proposed that false positive errors for medial meniscal tears could be because of inability of arthroscopy to detect them. They reviewed the video tapes of arthroscopies in their study and correlated them with MR findings. 11 They found that in 53% of their false positive cases, posterior horn of medial meniscus wasn’t visualized on arthroscopy. In our study however, we can not determine whether false positives for meniscal tears were due to healed tears or tears missed on arthroscopy. If we consider the arthroscopy as a gold standard for diagnosing meniscal tears, these false positive errors become unavoidable because MR sequences can not differentiate between a healed tear and acute tear.
Another published report stated that interpretational errors were the least common errors to occur and two most commonly missed tears on MR images are posterior horn of medial meniscus and peripheral tears of the lateral meniscus lying adjacent to the popliteal bursa.7
Equivocal errors in which interpreters of MR images don’t agree on a diagnosis could be a significant cause of errors. Arthur et al concluded that 39% of errors in his study about MR Diagnosis of Meniscal tears and analysis of cause of errors, were due to equivocal errors.7 A study done about MR images of knee showed a range of sensitivity of 74-88% depending on the observer.12
Our study included more population of males compared to females. This can be attributed to several factors including less presentation of female population with knee involvements to orthopaedic outpatient department, less labour work compared to male population and less involvement in sports activities.
Study conducted by Garneau et al found “substantial intra and interobserver variability” in the diagnosis of labral tear using MR images.13 Sensitivity for diagnosing herniated cervical disks varied from 79% to 91% among three observers while using gradient-echo MR imaging.14 The above 4 studies suggest that observer variation is a strong factor in determining the sensitivity of any imaging diagnostic test. An observer with greater experience will significantly reduce this observer variation.
This study may be limited by the relatively lower number of PCL and meniscal injuries, and would benefit from further investigation. One of the limitation of our study included only reporting from a single radiologist for MRI ordered which could lead to human error.
CONCLUSION
MRI has high sensitivity and NPV for ACLI & PCLI, low sensitivity for LMI, low specificity for MMI and low PPV for PCLI, MMI and LMI. In cases of clinical suspicion of meniscal or ligamental injury, clinicians should not rely on MRI findings alone but should follow it up with diagnostic arthroscopy.
REFERENCES
1. Barry KP, Mesgarzadeh M, Triolo J, Moyer R, Tehranzadeh J, Bonakdarpour A. Accuracy of MRI patterns in evaluating anterior cruciate ligament tears. Skeletal Radiol 1996;25(4):365-70. https://doi.org/10.1007/s002560050096
2. Barber-Westin SD, Noyes FR. Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Arthroscopy 2011;27(12):1697-705. https://doi.org/10.1016/j.arthro.2011.09.009
3. De Smet AA, Graf BK. Meniscal tears missed on MR imaging: relationship to meniscal tear patterns and anterior cruciate ligament tears. Am J Roentgenol 1994;162(4):905-11. https://doi.org/10.2214/ajr.162.4.8141016
4. Arnoldi AP, Weckbach S, Nussbickel C, Horng A, Nöbauer I, Zysk S, et al. [MRI based volumetric assessment of knee cartilage after ACL-reconstruction, correlated with qualitative morphologic changes in the joint and with clinical outcome. Is there evidence for early posttraumatic degeneration?]. Rofo 2011;183(12):1138-44. https://doi.org/10.1055/s-0031-1281685
5. Logan MC, Williams A, Lavelle J, Gedroyc W, Freeman M. Tibiofemoral kinematics following successful anterior cruciate ligament reconstruction using dynamic multiple resonance imaging. Am J Sports Med 2004;32(4):984-92. https://doi.org/10.1177/0363546503261702
6. Lee JK, Yao L, Phelps CT, Wirth CR, Czajka J, Lozman J. Anterior cruciate ligament tears: MR imaging compared with arthroscopy and clinical tests. Radiology 1988;166(3):861-4. https://doi.org/10.1148/radiology.166.3.3340785
7. De Smet AA, Tuite MJ, Norris MA, Swan JS. MR diagnosis of meniscal tears: analysis of causes of errors. Am J Roentgenol 1994;163(6):1419-23. https://doi.org/10.2214/ajr.163.6.7992739
8. Dandy DJ. The impact of arthroscopic surgery on the management of disorders of the knee. Arthroscopy 1990;6(2):96-9. https://doi.org/10.1016/0749-8063(90)90006-y
9. Quinn SF, Brown TF. Meniscal tears diagnosed with MR imaging versus arthroscopy: how reliable a standard is arthroscopy? Radiology 1991;181(3):843-7. https://doi.org/10.1148/radiology.181.3.1947108
10. Deutsch A, Mink J, Fox J, Arnoczky S, Rothman B, Stoller D, et al. Peripheral meniscal tears: MR findings after conservative treatment or arthroscopic repair. Radiology 1990;176(2):485-8. https://doi.org/10.1148/radiology.176.2.2367665
11.; Quinn SF, Brown TF. Meniscal tears diagnosed with MR imaging versus arthroscopy: how reliable a standard is arthroscopy? Radiology 1991;181(3):843-7. https://doi.org/10.1148/radiology.181.3.1947108
12. De Smet AA, Norris MA, Yandow DR, Graf BK, Keene JS. Diagnosis of meniscal tears of the knee with MR imaging: effect of observer variation and sample size on sensitivity and specificity. Am J Roentgenol 1993;160(3):555-9. https://doi.org/10.2214/ajr.160.3.8430552
13. Garneau RA, Renfrew DL, Moore TE, el-KhouryGY, Nepola JV, Lemke JH. Glenoid labrum: evaluation with MR imaging. Radiology 1991;179(2):519-22. https://doi.org/10.1148/radiology.179.2.2014303
14. Yousem DM, Atlas SW, Hackney DB. Cervical spine disk herniation: comparison of CT and 3DFT gradient echo MR scans. J Comput Assist Tomogr 1992;16(3):345-51.
|
Following authors have made substantial contributions to the manuscript as under:
QS: Acquisition of data, drafting the manuscript, approval of the final version to be published. OSK: Analysis and interpretation of data, drafting the manuscript, approval of the final version to be published QA: Concept and study design, acquisition of data, drafting the manuscript, critical review, approval of the final version to be published. AJM& ZA: Concept and study design, critical review, approval of the final version to be published.
Authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. |
|
CONFLICT OF INTEREST Authors declared no conflict of interest
GRANT SUPPORT AND FINANCIAL DISCLOSURE Authors declared no specific grant for this research from any funding agency in the public, commercial or non-profit sectors |
|
DATA SHARING STATEMENT The data that support the findings of this study are available from the corresponding author upon reasonable request |
|
This
is an Open Access article distributed under the terms of the Creative Commons
Attribution-Non-Commercial 2.0 Generic License. |
|
KMUJ web address: www.kmuj.kmu.edu.pk Email address: kmuj@kmu.edu.pk |